Monday Poster Session
Category: Biliary/Pancreas
P1734 - A Nationwide Comparison of the Outcomes of Endoscopic Versus Percutaneous Gallbladder Drainage in the Management of Acute Cholecystitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yassine Kilani, MD
SSM Health Saint Louis University Hospital
St. Louis, MO
Presenting Author(s)
Yassine Kilani, MD1, Mahmoud Y. Madi, MD1, Kym Yves Tan. Sirilan, MD2, Marina Kim, MD1, Antonio R. Cheesman, MD1
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2NYC Health + Hospitals/Lincoln, New York, NY
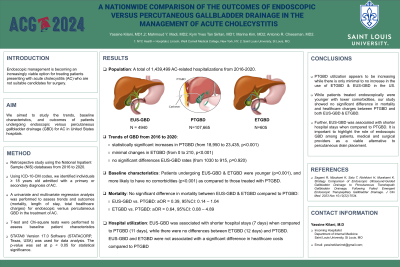
Introduction: Endoscopic management is becoming an increasingly viable option for treating patients presenting with acute cholecystitis (AC) who are not suitable candidates for surgery. We aimed to study the trends, baseline characteristics, and outcomes of patients undergoing endoscopic versus percutaneous gallbladder drainage (GBD) for AC in United States hospitals.
Methods: This is a retrospective longitudinal study of patients admitted with a primary or secondary diagnosis of AC. Data were obtained from the 2016 to 2020 Nationwide Inpatient Sample databases using International Classification of Disease codes (tenth revision, ICD-10). Univariate and multivariate regression analyses were performed to assess trends and outcomes (mortality, length of stay, total healthcare charges) for endoscopic versus percutaneous GBD in the treatment of AC. T-test and Chi-square tests were performed to assess baseline patient characteristics.
Results: A total of 1,439,499 adult patients were admitted with a diagnosis of AC. 11.0% underwent percutaneous transhepatic GBD (PTGBD), 0.5% had endoscopic ultrasound-guided GBD (EUS-GBD), and 0.06% endoscopic transpapillary GBD (ETGBD). Statistically significant increases in the rates of PTGBD (from 18,950 to 23,435, p< 0.001) were observed, while the rates of ETGBD showed minimal changes (from 0 to 210, p< 0.001), and EUS-GBD rates remained constant (from 1030 to 915, p=0.920) over the period of the study. Patients undergoing EUS-GBD and ETGBD were younger (Mean age - PTGBD: 71 years, EUS-GBD: 65 years, ETGBD: 68 years, p< 0.001), and more likely to have no comorbidities (PTGBD: 13.5%, EUS-GBD: 28.5%, ETGBD: 16.5%, p< 0.001) as compared to those treated with PTGBD. On multivariable regression analysis, treatment with EUS-GBD and ETGBD was not associated with a significant difference in mortality or healthcare costs compared to PTGBD (Table 1). Further, patients undergoing EUS-GBD had shorter hospital stays (7.38 days), as compared to those undergoing PTGBD (10.74 days; adjusted Mean Difference = -1.80 days, 95%CI: -2.94 – -0.66; Table 1).
Discussion: PTGBD utilization rate appears to be increasing while there is only minimal to no increase in the use of ETGBD and EUS-GBD in the US. While patients treated endoscopically were younger and appeared to have lower comorbidities, our study showed no significant difference in mortality and healthcare charges between PTGBD and both EUS-GBD and ETGBD. Further, EUS-GBD was associated with shorter hospital stays when compared to PTGBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yassine Kilani, MD1, Mahmoud Y. Madi, MD1, Kym Yves Tan. Sirilan, MD2, Marina Kim, MD1, Antonio R. Cheesman, MD1. P1734 - A Nationwide Comparison of the Outcomes of Endoscopic Versus Percutaneous Gallbladder Drainage in the Management of Acute Cholecystitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2NYC Health + Hospitals/Lincoln, New York, NY
Introduction: Endoscopic management is becoming an increasingly viable option for treating patients presenting with acute cholecystitis (AC) who are not suitable candidates for surgery. We aimed to study the trends, baseline characteristics, and outcomes of patients undergoing endoscopic versus percutaneous gallbladder drainage (GBD) for AC in United States hospitals.
Methods: This is a retrospective longitudinal study of patients admitted with a primary or secondary diagnosis of AC. Data were obtained from the 2016 to 2020 Nationwide Inpatient Sample databases using International Classification of Disease codes (tenth revision, ICD-10). Univariate and multivariate regression analyses were performed to assess trends and outcomes (mortality, length of stay, total healthcare charges) for endoscopic versus percutaneous GBD in the treatment of AC. T-test and Chi-square tests were performed to assess baseline patient characteristics.
Results: A total of 1,439,499 adult patients were admitted with a diagnosis of AC. 11.0% underwent percutaneous transhepatic GBD (PTGBD), 0.5% had endoscopic ultrasound-guided GBD (EUS-GBD), and 0.06% endoscopic transpapillary GBD (ETGBD). Statistically significant increases in the rates of PTGBD (from 18,950 to 23,435, p< 0.001) were observed, while the rates of ETGBD showed minimal changes (from 0 to 210, p< 0.001), and EUS-GBD rates remained constant (from 1030 to 915, p=0.920) over the period of the study. Patients undergoing EUS-GBD and ETGBD were younger (Mean age - PTGBD: 71 years, EUS-GBD: 65 years, ETGBD: 68 years, p< 0.001), and more likely to have no comorbidities (PTGBD: 13.5%, EUS-GBD: 28.5%, ETGBD: 16.5%, p< 0.001) as compared to those treated with PTGBD. On multivariable regression analysis, treatment with EUS-GBD and ETGBD was not associated with a significant difference in mortality or healthcare costs compared to PTGBD (Table 1). Further, patients undergoing EUS-GBD had shorter hospital stays (7.38 days), as compared to those undergoing PTGBD (10.74 days; adjusted Mean Difference = -1.80 days, 95%CI: -2.94 – -0.66; Table 1).
Discussion: PTGBD utilization rate appears to be increasing while there is only minimal to no increase in the use of ETGBD and EUS-GBD in the US. While patients treated endoscopically were younger and appeared to have lower comorbidities, our study showed no significant difference in mortality and healthcare charges between PTGBD and both EUS-GBD and ETGBD. Further, EUS-GBD was associated with shorter hospital stays when compared to PTGBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yassine Kilani indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Kym Yves Sirilan indicated no relevant financial relationships.
Marina Kim indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Yassine Kilani, MD1, Mahmoud Y. Madi, MD1, Kym Yves Tan. Sirilan, MD2, Marina Kim, MD1, Antonio R. Cheesman, MD1. P1734 - A Nationwide Comparison of the Outcomes of Endoscopic Versus Percutaneous Gallbladder Drainage in the Management of Acute Cholecystitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
