Monday Poster Session
Category: Biliary/Pancreas
P1738 - Is There an Association Between Quality Of Life And The Amount Of Pain Medications That Chronic Pancreatitis Patients Are Taking?
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- TP
Thin Phyu Phyu Aung, MD
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Thin Phyu Phyu Aung, MD, Yong Eun, MD, Mohamed K.. Osman, MD, MPH, Joan Culpepper-Morgan, MD, FACG
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Pain in chronic pancreatitis (CP) is distressing, disruptive, debilitating, and affects quality of life (QoL). CP patients may be prescribed pancrealipase, opioid and/or non-opioid medications for pain management, all with variable and some with doubtful efficacy. This study aimed to quantify pain control and Qol in CP patients, and to determine if there was any association with the numbers of medications they were taking.
Methods: We analyzed data from 239,757 participants in the United States using the All of Us database. After exclusion of those without gender information or survey data, we defined CP using ICD-9/10 codes, and participants without the diagnosis of CP were used as the reference group. Medication history for pancrealipase, opioid, and non-opioid medication use were analyzed. We compared demographic profiles, QoL and pain scores between CP and non-CP patients using survey data. We also did subgroup analyses to determine if there was any difference in QoL and pain scores between patients receiving one, two, or three types of medications. Welch Two Sample t-test, One-Way ANOVA test, and paired t-test were used for analysis, using the R programming language.
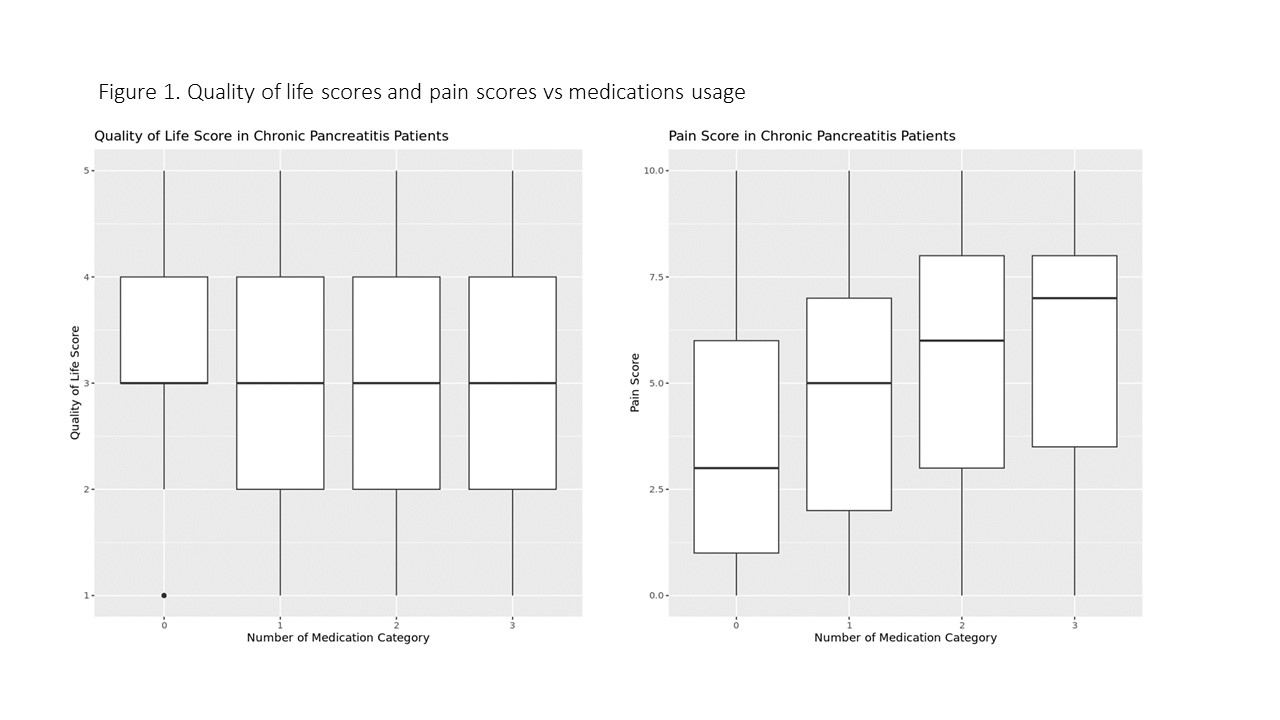
Results: We identified 1846 participants with CP leaving 237,911 participants as non-CP controls. The mean age of the CP patients was 59. Most, 51.8% were female. The race/ethnicity make-up of the two groups was similar except for greater representation of Non-Hispanic Blacks in the CP group (23.4% vs 19.3%) as well as fewer Non-Hispanic Whites (52.5% vs 55.2%). A significantly greater percentage of CP subjects were normal weight (33.4% vs 26.8%) or underweight (6.4% vs 1.6%) compared to the controls. Few (4%) CP patients were taking pancrealipase, while 90% of them were taking either opioid or non-opioid medications. Overall, QoL scores were significantly worse for CP patients than controls 3.02± 1.07 vs 3.53± 1.02, p< 0.001. Likewise, pain scores were also significantly higher for CP patients than controls 5.26± 3.07 vs 3.29± 2.96, p< 0.001. When divided into groups taking no meds, one or two, more than two meds, 83.4% of CP patients were taking two types of medication. More medication was associated with higher pain scores but not with QoL scores (Table 1, Figure 1).
Discussion: CP patients seem to have a worse QoL associated with increased pain. Unfortunately, stepwise increase in pain medications does not seem to improve the QoL. Better treatments are clearly needed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Thin Phyu Phyu Aung, MD, Yong Eun, MD, Mohamed K.. Osman, MD, MPH, Joan Culpepper-Morgan, MD, FACG. P1738 - Is There an Association Between Quality Of Life And The Amount Of Pain Medications That Chronic Pancreatitis Patients Are Taking?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYC Health + Hospitals/Harlem, New York, NY
Introduction: Pain in chronic pancreatitis (CP) is distressing, disruptive, debilitating, and affects quality of life (QoL). CP patients may be prescribed pancrealipase, opioid and/or non-opioid medications for pain management, all with variable and some with doubtful efficacy. This study aimed to quantify pain control and Qol in CP patients, and to determine if there was any association with the numbers of medications they were taking.
Methods: We analyzed data from 239,757 participants in the United States using the All of Us database. After exclusion of those without gender information or survey data, we defined CP using ICD-9/10 codes, and participants without the diagnosis of CP were used as the reference group. Medication history for pancrealipase, opioid, and non-opioid medication use were analyzed. We compared demographic profiles, QoL and pain scores between CP and non-CP patients using survey data. We also did subgroup analyses to determine if there was any difference in QoL and pain scores between patients receiving one, two, or three types of medications. Welch Two Sample t-test, One-Way ANOVA test, and paired t-test were used for analysis, using the R programming language.
Results: We identified 1846 participants with CP leaving 237,911 participants as non-CP controls. The mean age of the CP patients was 59. Most, 51.8% were female. The race/ethnicity make-up of the two groups was similar except for greater representation of Non-Hispanic Blacks in the CP group (23.4% vs 19.3%) as well as fewer Non-Hispanic Whites (52.5% vs 55.2%). A significantly greater percentage of CP subjects were normal weight (33.4% vs 26.8%) or underweight (6.4% vs 1.6%) compared to the controls. Few (4%) CP patients were taking pancrealipase, while 90% of them were taking either opioid or non-opioid medications. Overall, QoL scores were significantly worse for CP patients than controls 3.02± 1.07 vs 3.53± 1.02, p< 0.001. Likewise, pain scores were also significantly higher for CP patients than controls 5.26± 3.07 vs 3.29± 2.96, p< 0.001. When divided into groups taking no meds, one or two, more than two meds, 83.4% of CP patients were taking two types of medication. More medication was associated with higher pain scores but not with QoL scores (Table 1, Figure 1).
Discussion: CP patients seem to have a worse QoL associated with increased pain. Unfortunately, stepwise increase in pain medications does not seem to improve the QoL. Better treatments are clearly needed.
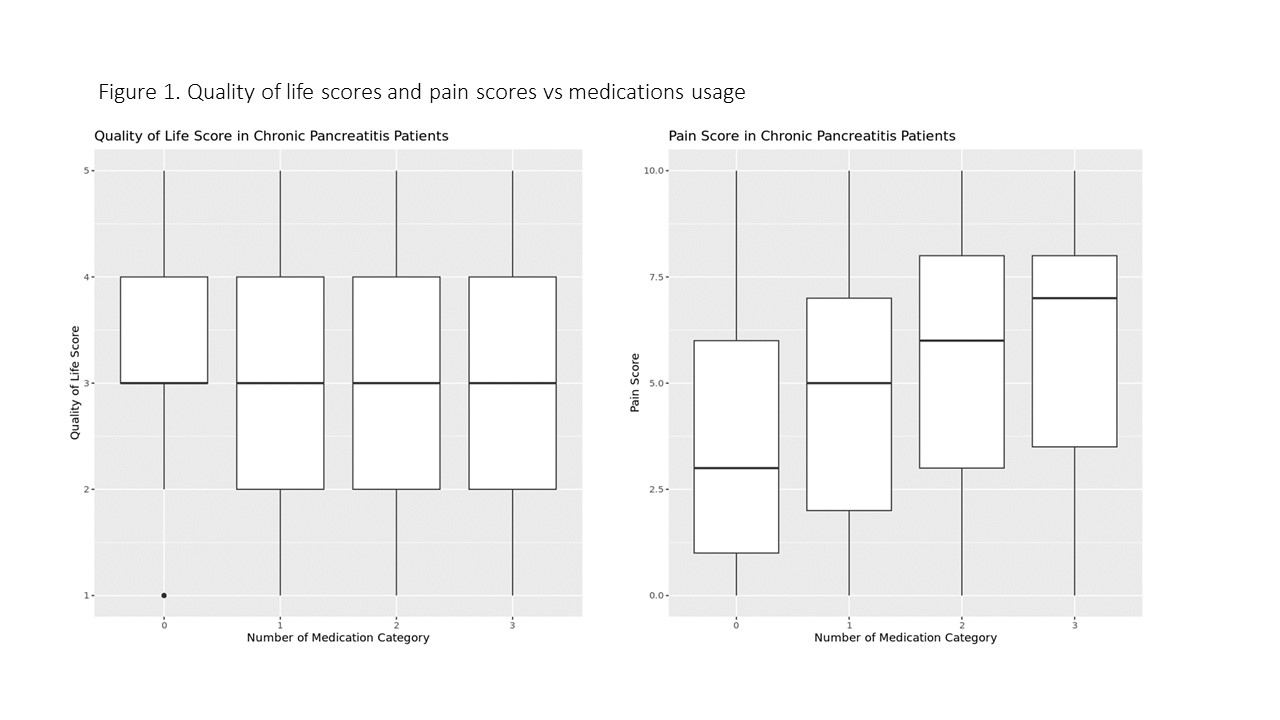
Figure: Figure 1- Quality of life scores and pain scores Vs medication usage
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Thin Phyu Phyu Aung indicated no relevant financial relationships.
Yong Eun indicated no relevant financial relationships.
Mohamed Osman indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Thin Phyu Phyu Aung, MD, Yong Eun, MD, Mohamed K.. Osman, MD, MPH, Joan Culpepper-Morgan, MD, FACG. P1738 - Is There an Association Between Quality Of Life And The Amount Of Pain Medications That Chronic Pancreatitis Patients Are Taking?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
