Monday Poster Session
Category: Biliary/Pancreas
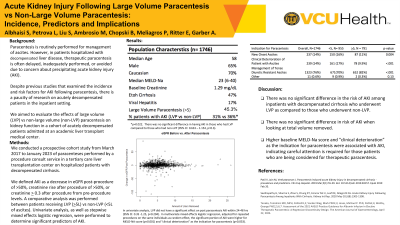
P1750 - Acute Kidney Injury Following Large Volume Paracentesis vs Non-Large Volume Paracentesis: Incidence, Predictors and Implications
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Somaya Albhaisi, MBBCh, MPH
Virginia Commonwealth University
Pasadena, CA
Presenting Author(s)
Somaya Albhaisi, MBBCh, MPH, Lana Petrova, BS, Stanley Liu, MD, Matthew Ambrosio, MS, Benjamin Chopski, DO, Pete Meliagros, MD, Evan Ritter, MD, Adam Garber, MD
Virginia Commonwealth University, Richmond, VA
Introduction: Despite existing research on acute kidney injury (AKI) incidence following paracentesis, there is limited research on acutely decompensated inpatients. Our study aimed to evaluate the effects of large volume (LVP) vs non-large volume (non-LVP) paracentesis on kidney function in a cohort of acutely decompensated cirrhosis patients admitted at an academic liver transplant medical center.
Methods: We conducted a prospective cohort study (2017-2023) of paracenteses performed by a medicine procedure service in a tertiary care transplant center on hospitalized patients with decompensated cirrhosis. AKI was defined as a decrease in eGFR post-procedure of >50%, creatinine rise post-procedure of >50%, or creatinine >0.3 post-procedure from pre-procedure levels. We compared patients receiving LVP ( >5L) vs non-LVP (<5L). Univariate analysis and stepwise mixed effects logistic regression were performed to identify AKI predictors.
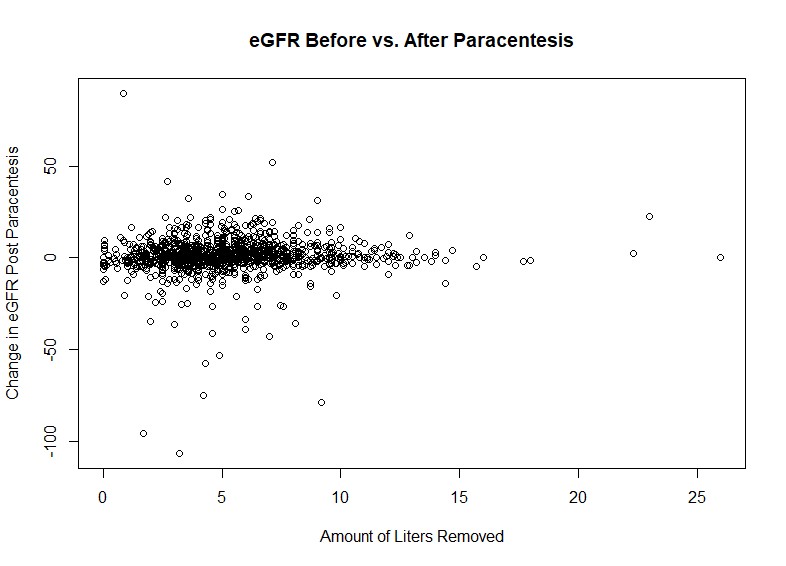
Results: A total of 1,746 patients underwent paracenteses during the study period. Most of the paracenteses (54.7%) were non-LVP. The median age of the entire cohort was 58 years, 65% were male, and 70% were Caucasian race. The median baseline creatinine and MELD-Na score were 1.29 mg/dl and 23, respectively. The most common etiology of cirrhosis was alcohol-associated (47%), followed by viral hepatitis (17%) (Table 1). AKI was observed in 247 (31%) patients who underwent LVP, and 348 (36%) patients who underwent non-LVP (p=0.022). There was no significant difference in the odds of having AKI in those who had LVP compared to those who had non-LVP (95% CI: 0.633-1.154, p=0.3). In univariate analysis, LVP did not have a significant effect on post paracentesis AKI. In multivariate mixed effect logistic regression, adjusted for repeated procedures on the same individuals as a random effect, the significant predictors of AKI were higher MELD-Na score (p< 0.001) and “clinical deterioration” as the indication for paracentesis (p=0.033). The total volume of ascitic fluid removed was not associated with a statistically significant change in eGFR (Figure 1).
Discussion: There was no significant difference in the risk of AKI or change in eGFR with volume removed among inpatients with decompensated cirrhosis who underwent LVP as compared to those who underwent non-LVP. Higher baseline MELD-Na score and clinical deterioration were associated with AKI, indicating that careful attention is required for those patients who are being considered for therapeutic paracentesis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Somaya Albhaisi, MBBCh, MPH, Lana Petrova, BS, Stanley Liu, MD, Matthew Ambrosio, MS, Benjamin Chopski, DO, Pete Meliagros, MD, Evan Ritter, MD, Adam Garber, MD. P1750 - Acute Kidney Injury Following Large Volume Paracentesis vs Non-Large Volume Paracentesis: Incidence, Predictors and Implications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Virginia Commonwealth University, Richmond, VA
Introduction: Despite existing research on acute kidney injury (AKI) incidence following paracentesis, there is limited research on acutely decompensated inpatients. Our study aimed to evaluate the effects of large volume (LVP) vs non-large volume (non-LVP) paracentesis on kidney function in a cohort of acutely decompensated cirrhosis patients admitted at an academic liver transplant medical center.
Methods: We conducted a prospective cohort study (2017-2023) of paracenteses performed by a medicine procedure service in a tertiary care transplant center on hospitalized patients with decompensated cirrhosis. AKI was defined as a decrease in eGFR post-procedure of >50%, creatinine rise post-procedure of >50%, or creatinine >0.3 post-procedure from pre-procedure levels. We compared patients receiving LVP ( >5L) vs non-LVP (<5L). Univariate analysis and stepwise mixed effects logistic regression were performed to identify AKI predictors.
Results: A total of 1,746 patients underwent paracenteses during the study period. Most of the paracenteses (54.7%) were non-LVP. The median age of the entire cohort was 58 years, 65% were male, and 70% were Caucasian race. The median baseline creatinine and MELD-Na score were 1.29 mg/dl and 23, respectively. The most common etiology of cirrhosis was alcohol-associated (47%), followed by viral hepatitis (17%) (Table 1). AKI was observed in 247 (31%) patients who underwent LVP, and 348 (36%) patients who underwent non-LVP (p=0.022). There was no significant difference in the odds of having AKI in those who had LVP compared to those who had non-LVP (95% CI: 0.633-1.154, p=0.3). In univariate analysis, LVP did not have a significant effect on post paracentesis AKI. In multivariate mixed effect logistic regression, adjusted for repeated procedures on the same individuals as a random effect, the significant predictors of AKI were higher MELD-Na score (p< 0.001) and “clinical deterioration” as the indication for paracentesis (p=0.033). The total volume of ascitic fluid removed was not associated with a statistically significant change in eGFR (Figure 1).
Discussion: There was no significant difference in the risk of AKI or change in eGFR with volume removed among inpatients with decompensated cirrhosis who underwent LVP as compared to those who underwent non-LVP. Higher baseline MELD-Na score and clinical deterioration were associated with AKI, indicating that careful attention is required for those patients who are being considered for therapeutic paracentesis.
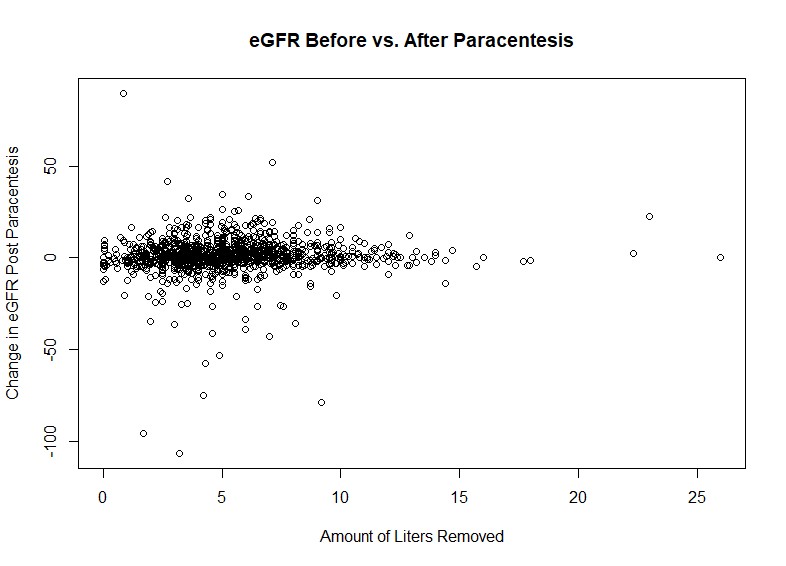
Figure: Figure 1. Correlation between changes in eGFR and volume of ascitic fluid removed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Somaya Albhaisi indicated no relevant financial relationships.
Lana Petrova indicated no relevant financial relationships.
Stanley Liu indicated no relevant financial relationships.
Matthew Ambrosio indicated no relevant financial relationships.
Benjamin Chopski indicated no relevant financial relationships.
Pete Meliagros indicated no relevant financial relationships.
Evan Ritter indicated no relevant financial relationships.
Adam Garber indicated no relevant financial relationships.
Somaya Albhaisi, MBBCh, MPH, Lana Petrova, BS, Stanley Liu, MD, Matthew Ambrosio, MS, Benjamin Chopski, DO, Pete Meliagros, MD, Evan Ritter, MD, Adam Garber, MD. P1750 - Acute Kidney Injury Following Large Volume Paracentesis vs Non-Large Volume Paracentesis: Incidence, Predictors and Implications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

