Monday Poster Session
Category: Biliary/Pancreas
P1755 - Association of Elevated Liver Biochemistries and Clinical Outcomes Within Strata of Alkaline Phosphatase Levels in Patients With Primary Biliary Cholangitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DW
Darren Wheeler, PhD
Intercept Pharmaceuticals, Inc.
Morristown, NJ
Presenting Author(s)
David W. Victor, MD1, Joanna P. MacEwan, PhD2, Jennifer Hernandez, MS2, Radhika Nair, PhD3, Mustafa Kamal, PharmD, RPh3, Darren Wheeler, PhD3, Jing Li, PhD3, Leona Bessonova, PhD3, Christopher Gasink, MD3, Kris V.. Kowdley, MD, FACG4
1Houston Methodist Hospital, Houston, TX; 2Genesis Research Group, Hoboken, NJ; 3Intercept Pharmaceuticals, Inc., Morristown, NJ; 4Liver Institute Northwest, Seattle, WA
Introduction: In patients (pts) with primary biliary cholangitis (PBC), elevated liver tests and their duration correlate with increased risk of negative outcomes. We assessed the relationship between the degree of elevation of liver tests (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]) and fibrosis scores (fibrosis-4 [FIB-4] and AST/platelet ratio index [APRI]) in various alkaline phosphatase (ALP) strata.
Methods: Pts ≥ 18 years old with ≥ 1 inpatient or ≥ 2 outpatient PBC claims between July 2014 and February 2022 were identified from Komodo Health merged with national lab data, with the date of the first claim as the index date. Pts with ≥ 1 measurement of ALP, total bilirubin, ALT, and AST during the pre-index period (6 months before and including index date), and ≥ 1 post-index measurement were stratified into 3 groups based on baseline ALP levels. Within each ALP stratum, a multivariable Cox proportional hazards model assessed the association between a time-varying covariate and the composite endpoint (hospitalization for hepatic decompensation, liver transplant, or death). Within each ALP stratum, separate models were run for each biomarker and fibrosis score. Pts were censored at initiation of second-line therapy, end of enrollment, or end of follow-up.
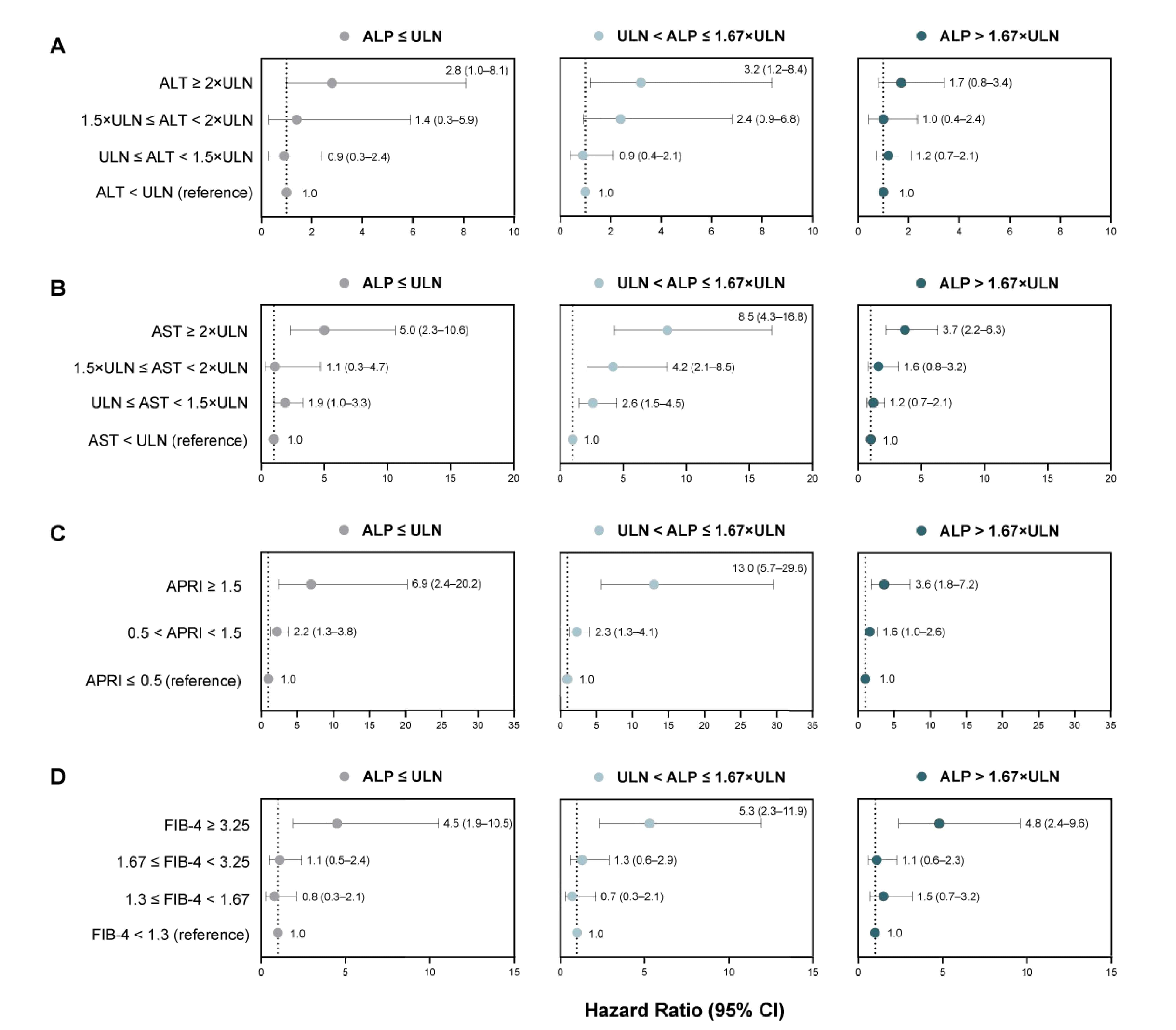
Results: A total of 3974 pts were stratified into 3 groups: ALP ≤ ULN (n=1443), ALP >ULN to ≤ 1.67×ULN (n=1279), and ALP > 1.67×ULN (n=1252). Across ALP strata (Fig. 1), pts with FIB-4 ≥ 3.25 and APRI > 0.5 had increased risk of negative hepatic outcomes compared to pts with FIB-4 < 1.3 and APRI ≤ 0.5, respectively (hazard ratio (HR [95% CI]) range: 4.5 [1.9-10.5] to 5.3 [2.3-11.9] and 1.6 [1.0-2.6] to 13.0 [5.7-29.6]). Compared with pts with AST < ULN, those with AST ≥ 2.0×ULN generally had increased risk of negative hepatic outcomes across ALP strata (HR [95% CI] range: 3.7 [2.2-6.3] to 8.5 [4.3-16.8]). Among pts with baseline ALP ≤ 1.67×ULN, pts with ALT ≥ 2×ULN had higher risk of negative hepatic outcomes compared to pts with ALT < ULN (HR [95% CI] range: 2.8 [1.0-8.1] to 3.2 [1.2-8.4]).
Discussion: Irrespective of ALP strata, even when ALP is < ULN, elevated biomarkers and fibrosis scores were associated with increased risk of hospitalization for hepatic decompensation, liver transplant, or death, highlighting the importance of comprehensive and timely monitoring and treatment of pts with PBC.
©2023 Komodo Health, Inc. All rights reserved. Used with permission.
Disclosures:
David W. Victor, MD1, Joanna P. MacEwan, PhD2, Jennifer Hernandez, MS2, Radhika Nair, PhD3, Mustafa Kamal, PharmD, RPh3, Darren Wheeler, PhD3, Jing Li, PhD3, Leona Bessonova, PhD3, Christopher Gasink, MD3, Kris V.. Kowdley, MD, FACG4. P1755 - Association of Elevated Liver Biochemistries and Clinical Outcomes Within Strata of Alkaline Phosphatase Levels in Patients With Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Houston Methodist Hospital, Houston, TX; 2Genesis Research Group, Hoboken, NJ; 3Intercept Pharmaceuticals, Inc., Morristown, NJ; 4Liver Institute Northwest, Seattle, WA
Introduction: In patients (pts) with primary biliary cholangitis (PBC), elevated liver tests and their duration correlate with increased risk of negative outcomes. We assessed the relationship between the degree of elevation of liver tests (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]) and fibrosis scores (fibrosis-4 [FIB-4] and AST/platelet ratio index [APRI]) in various alkaline phosphatase (ALP) strata.
Methods: Pts ≥ 18 years old with ≥ 1 inpatient or ≥ 2 outpatient PBC claims between July 2014 and February 2022 were identified from Komodo Health merged with national lab data, with the date of the first claim as the index date. Pts with ≥ 1 measurement of ALP, total bilirubin, ALT, and AST during the pre-index period (6 months before and including index date), and ≥ 1 post-index measurement were stratified into 3 groups based on baseline ALP levels. Within each ALP stratum, a multivariable Cox proportional hazards model assessed the association between a time-varying covariate and the composite endpoint (hospitalization for hepatic decompensation, liver transplant, or death). Within each ALP stratum, separate models were run for each biomarker and fibrosis score. Pts were censored at initiation of second-line therapy, end of enrollment, or end of follow-up.
Results: A total of 3974 pts were stratified into 3 groups: ALP ≤ ULN (n=1443), ALP >ULN to ≤ 1.67×ULN (n=1279), and ALP > 1.67×ULN (n=1252). Across ALP strata (Fig. 1), pts with FIB-4 ≥ 3.25 and APRI > 0.5 had increased risk of negative hepatic outcomes compared to pts with FIB-4 < 1.3 and APRI ≤ 0.5, respectively (hazard ratio (HR [95% CI]) range: 4.5 [1.9-10.5] to 5.3 [2.3-11.9] and 1.6 [1.0-2.6] to 13.0 [5.7-29.6]). Compared with pts with AST < ULN, those with AST ≥ 2.0×ULN generally had increased risk of negative hepatic outcomes across ALP strata (HR [95% CI] range: 3.7 [2.2-6.3] to 8.5 [4.3-16.8]). Among pts with baseline ALP ≤ 1.67×ULN, pts with ALT ≥ 2×ULN had higher risk of negative hepatic outcomes compared to pts with ALT < ULN (HR [95% CI] range: 2.8 [1.0-8.1] to 3.2 [1.2-8.4]).
Discussion: Irrespective of ALP strata, even when ALP is < ULN, elevated biomarkers and fibrosis scores were associated with increased risk of hospitalization for hepatic decompensation, liver transplant, or death, highlighting the importance of comprehensive and timely monitoring and treatment of pts with PBC.
©2023 Komodo Health, Inc. All rights reserved. Used with permission.
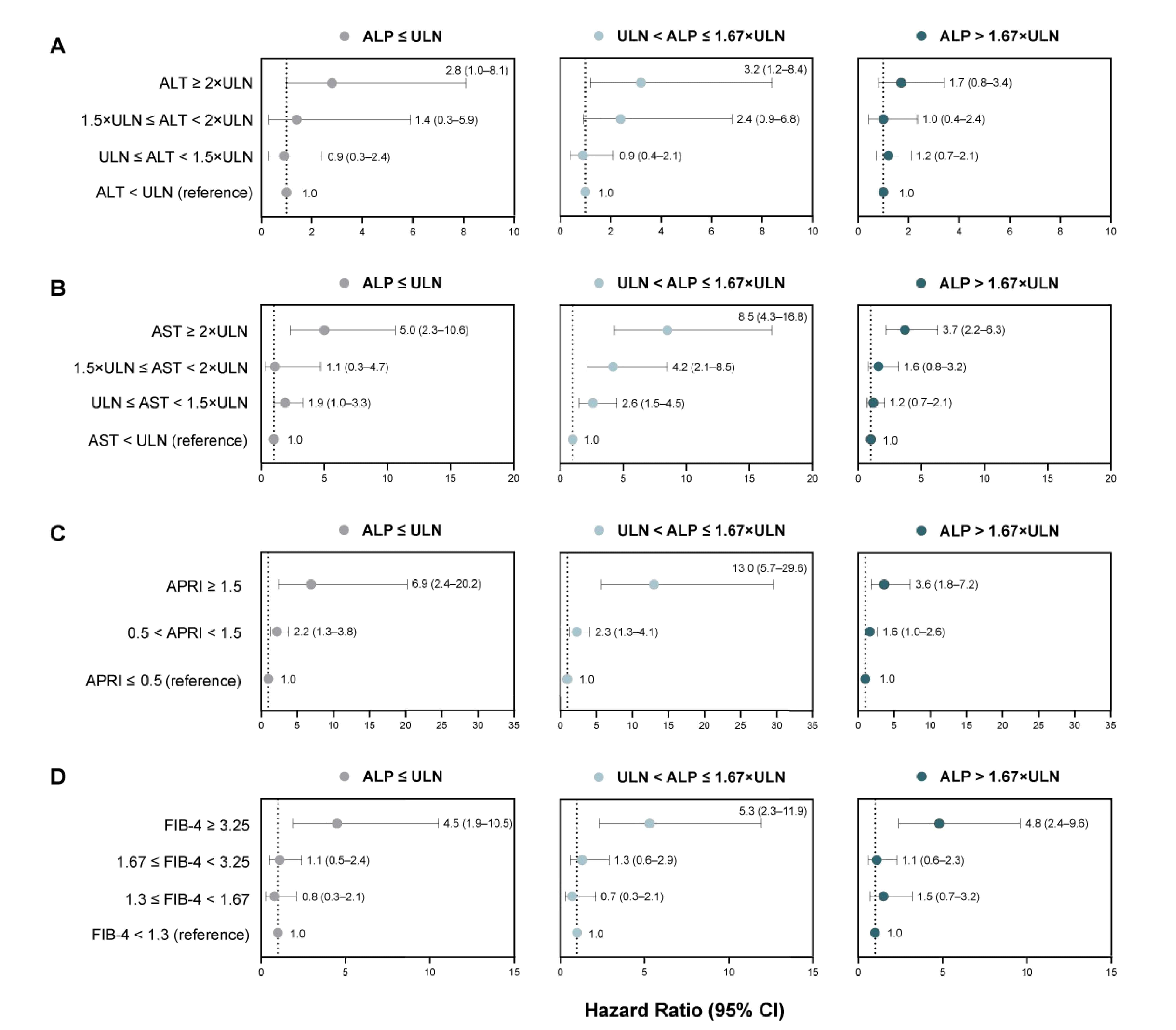
Figure: Figure 1. Hazard ratios of a composite endpoint (hospitalization for hepatic decompensation, liver transplant, or death) among patients with PBC for different thresholds of FIB-4 (A), APRI (B), AST (C), and ALT (D) in 3 ALP strata.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; APRI, aspartate aminotransferase to platelet ratio index; AST, aspartate aminotransferase; CI, confidence interval; FIB-4, fibrosis-4; PBC, primary biliary cholangitis; ULN, upper limit of normal.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; APRI, aspartate aminotransferase to platelet ratio index; AST, aspartate aminotransferase; CI, confidence interval; FIB-4, fibrosis-4; PBC, primary biliary cholangitis; ULN, upper limit of normal.
Disclosures:
David Victor: Gilead – speaker fees. Intercept Pharmaceuticals, Inc. – Advisory Committee/Board Member, Consultant, Speaker fees. Sebela – Consultant.
Joanna MacEwan: Genesis Research Group – Employee.
Jennifer Hernandez: Genesis Research Group – Employee.
Radhika Nair: Intercept Pharmaceuticals, Inc. – Employee.
Mustafa Kamal: Intercept Pharmaceuticals, Inc. – Employee.
Darren Wheeler: Intercept Pharmaceuticals, Inc. – Employee.
Jing Li: Intercept Pharmaceuticals Inc. – Employee.
Leona Bessonova: Intercept Pharmaceuticals, Inc. – Employee.
Christopher Gasink: Intercept Pharmaceuticals, Inc. – Employee. Johnson & Johnson – Employee.
Kris Kowdley: 89bio – Consultant, Grant/Research Support. AbbVie – Consultant, Grant/Research Support. Boston Pharmaceuticals – Consultant, Grant/Research Support. CymaBay, a Gilead Sciences Company – Consultant, Grant/Research Support. Enanta – Consultant, Grant/Research Support. Genfit – Consultant, Grant/Research Support. Gilead Sciences, Inc. – Consultant, Grant/Research Support. Hanmi – Consultant, Grant/Research Support. HighTide – Consultant, Grant/Research Support. Intercept – Consultant, Grant/Research Support. Ipsen – Consultant, Grant/Research Support. Madrigal – Consultant, Grant/Research Support. NGM – Consultant, Grant/Research Support. Novo Nordisk – Consultant, Grant/Research Support. TERNS – Consultant, Grant/Research Support. Viking – Consultant, Grant/Research Support.
David W. Victor, MD1, Joanna P. MacEwan, PhD2, Jennifer Hernandez, MS2, Radhika Nair, PhD3, Mustafa Kamal, PharmD, RPh3, Darren Wheeler, PhD3, Jing Li, PhD3, Leona Bessonova, PhD3, Christopher Gasink, MD3, Kris V.. Kowdley, MD, FACG4. P1755 - Association of Elevated Liver Biochemistries and Clinical Outcomes Within Strata of Alkaline Phosphatase Levels in Patients With Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
