Monday Poster Session
Category: Biliary/Pancreas
P1770 - Idiopathic Pancreatitis: Is the Glass Half Full?
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Yash R. Shah, MD
Trinity Health Oakland / Wayne State University School of Medicine
Pontiac, MI
Presenting Author(s)
Yash R. Shah, MD1, Adishwar Rao, MD2, Dushyant S. Dahiya, MD3, Hassam Ali, MD4, Manesh Kumar Gangwani, MD5, Saurabh Chandan, MD6, Angad Tiwari, MBBS7, Anupam Sule, MD1, Brian Markle, MD8, Geetha Krishnamoorthy, MD1, Mihaela Batke, MD9
1Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 2Guthrie Robert Packer Hospital, Fort Drum, NY; 3The University of Kansas School of Medicine, Kansas City, KS; 4ECU Health Medical Center, Greenville, NC; 5University of Toledo, Toledo, OH; 6CHI Health Creighton University Medical Center, Omaha, NE; 7Maharani Laxmi Bai Medical College, Jhansi, Uttar Pradesh, India; 8Trinity Health Oakland Hospital, Pontiac, MI; 9Trinity Health Oakland Hospital, Pontaic, MI
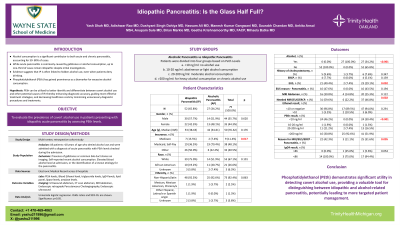
Introduction: Idiopathic pancreatitis (IP) presents diagnostic challenges, and often results in extensive diagnostic work-ups to identify etiology, including costly and potentially invasive procedures like Endoscopic Ultrasound (EUS), Endoscopic Retrograde Cholangiopancreatography (ERCP), and Magnetic Resonance Imaging (MRI). Phosphatidylethanol (PEth) is a reliable biomarker for chronic alcohol use. Our study aimed to evaluate the incidence of high PEth levels, reflecting covert alcohol use as the etiology of presumed IP.
Methods: This retrospective multicenter study included 79 patients diagnosed with pancreatitis: 52 with IP and 27 with alcoholic pancreatitis (AP) with PEth levels available. We collected demographic data, reported alcohol use, diagnostic imaging, and laboratory results, including ethanol levels. The primary aim was to assess covert alcohol use in patients with presumed IP. Secondary aim was to compare resource utilization for diagnostic testing in patients with IP versus AP.
Results: There were 55.7% males and 44.3% females with a median age of 50 years (IQR: 35-62). The proportion of African American patients was significantly higher in the AP group (40.7% vs. 19.2%, p=0.101). 53.9% (1.9% between 10-20, 21.2% between 20-200, and 30.8% with >200) of the patients with presumed IP had elevated PEth levels ( >20 ng/mL), suggesting chronic alcohol use. 100% of the patients with AP had elevated PEth levels. Ethanol levels were negative in 96.8% of IP and 89.5% in AP. IP patients had higher diagnostic procedure rates than AP patients (EUS: 40.4% vs. 7.4%, p=0.002; MRI: 30.8% vs. 14.8%, p=0.122). Advanced imaging (MRI/EUS/ERCP) was more frequently needed in IP patients (59.6% vs. 22.2%, p=0.002) (Table 1).
Discussion: A striking percentage (51.9%) of patients with presumed IP had an elevated PEth consistent with chronic alcohol use. Resource utilization for diagnostics testing was significantly higher in patients with presumed IP, both for standard imaging (US/CT) and advanced imaging (MRCP/EUS/ERCP).
Based on this results we suggest that PEth testing should be included in the initial diagnostic protocol for patients with idiopathic pancreatitis who deny alcohol use. Conversion of a diagnosis of IP to AP will likely result in improved patient care and significant cost savings by avoiding unnecessary diagnostic workup.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yash R. Shah, MD1, Adishwar Rao, MD2, Dushyant S. Dahiya, MD3, Hassam Ali, MD4, Manesh Kumar Gangwani, MD5, Saurabh Chandan, MD6, Angad Tiwari, MBBS7, Anupam Sule, MD1, Brian Markle, MD8, Geetha Krishnamoorthy, MD1, Mihaela Batke, MD9. P1770 - Idiopathic Pancreatitis: Is the Glass Half Full?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 2Guthrie Robert Packer Hospital, Fort Drum, NY; 3The University of Kansas School of Medicine, Kansas City, KS; 4ECU Health Medical Center, Greenville, NC; 5University of Toledo, Toledo, OH; 6CHI Health Creighton University Medical Center, Omaha, NE; 7Maharani Laxmi Bai Medical College, Jhansi, Uttar Pradesh, India; 8Trinity Health Oakland Hospital, Pontiac, MI; 9Trinity Health Oakland Hospital, Pontaic, MI
Introduction: Idiopathic pancreatitis (IP) presents diagnostic challenges, and often results in extensive diagnostic work-ups to identify etiology, including costly and potentially invasive procedures like Endoscopic Ultrasound (EUS), Endoscopic Retrograde Cholangiopancreatography (ERCP), and Magnetic Resonance Imaging (MRI). Phosphatidylethanol (PEth) is a reliable biomarker for chronic alcohol use. Our study aimed to evaluate the incidence of high PEth levels, reflecting covert alcohol use as the etiology of presumed IP.
Methods: This retrospective multicenter study included 79 patients diagnosed with pancreatitis: 52 with IP and 27 with alcoholic pancreatitis (AP) with PEth levels available. We collected demographic data, reported alcohol use, diagnostic imaging, and laboratory results, including ethanol levels. The primary aim was to assess covert alcohol use in patients with presumed IP. Secondary aim was to compare resource utilization for diagnostic testing in patients with IP versus AP.
Results: There were 55.7% males and 44.3% females with a median age of 50 years (IQR: 35-62). The proportion of African American patients was significantly higher in the AP group (40.7% vs. 19.2%, p=0.101). 53.9% (1.9% between 10-20, 21.2% between 20-200, and 30.8% with >200) of the patients with presumed IP had elevated PEth levels ( >20 ng/mL), suggesting chronic alcohol use. 100% of the patients with AP had elevated PEth levels. Ethanol levels were negative in 96.8% of IP and 89.5% in AP. IP patients had higher diagnostic procedure rates than AP patients (EUS: 40.4% vs. 7.4%, p=0.002; MRI: 30.8% vs. 14.8%, p=0.122). Advanced imaging (MRI/EUS/ERCP) was more frequently needed in IP patients (59.6% vs. 22.2%, p=0.002) (Table 1).
Discussion: A striking percentage (51.9%) of patients with presumed IP had an elevated PEth consistent with chronic alcohol use. Resource utilization for diagnostics testing was significantly higher in patients with presumed IP, both for standard imaging (US/CT) and advanced imaging (MRCP/EUS/ERCP).
Based on this results we suggest that PEth testing should be included in the initial diagnostic protocol for patients with idiopathic pancreatitis who deny alcohol use. Conversion of a diagnosis of IP to AP will likely result in improved patient care and significant cost savings by avoiding unnecessary diagnostic workup.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yash Shah indicated no relevant financial relationships.
Adishwar Rao indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Angad Tiwari indicated no relevant financial relationships.
Anupam Sule indicated no relevant financial relationships.
Brian Markle indicated no relevant financial relationships.
Geetha Krishnamoorthy indicated no relevant financial relationships.
Mihaela Batke indicated no relevant financial relationships.
Yash R. Shah, MD1, Adishwar Rao, MD2, Dushyant S. Dahiya, MD3, Hassam Ali, MD4, Manesh Kumar Gangwani, MD5, Saurabh Chandan, MD6, Angad Tiwari, MBBS7, Anupam Sule, MD1, Brian Markle, MD8, Geetha Krishnamoorthy, MD1, Mihaela Batke, MD9. P1770 - Idiopathic Pancreatitis: Is the Glass Half Full?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

