Monday Poster Session
Category: Biliary/Pancreas
P1810 - The Ultimate Run: Acute Pancreatitis as the Debut of Systemic Lupus Erythematosus (SLE)
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

José M. Bretón, MD
University of Puerto Rico, Medical Sciences Campus
San Juan, PR
Presenting Author(s)
José M.. Bretón, MD, José M. Hernández, MD, Paola N. Laracuente, MD, Tania M. Aguila, MD, Mark A. Vergara, MD
University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
Introduction: SLE is an autoimmune disease that affects multiple organ systems. The majority of patients will debut with musculoskeletal and dermatological manifestations. However, the gastrointestinal system is less likely to be involved, with symptoms occurring in half of cases. Occasionally, pancreatitis can occur as a rare complication, with an incidence rate of up to 8.2%. Typically, it manifests as widespread flare-ups in individuals already diagnosed, making its occurrence as the initial presentation exceedingly unusual. In fact, only limited number of cases have been documented in the literature where pancreatitis precedes SLE diagnosis.
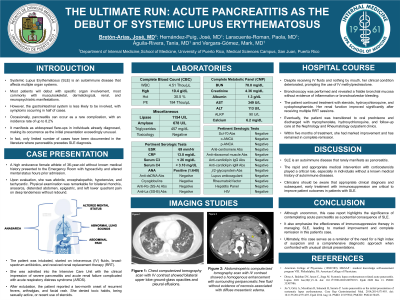
Case Description/Methods: A 36-year-old female athlete presented with hypoactivity and altered mental status. Upon evaluation, she was hypotensive, tachycardic and encephalopathic. Physical exam revealed a distended abdomen associated with epigastric, and left lower quadrant pain on deep tenderness without rebound. Laboratories revealed neutrophilia, bandemia, anemia, hypoalbuminemia, hypocalcemia, negative toxicology, normal triglycerides, and elevated inflammatory markers, amylase, and lipase. Imaging studies showed a homogenous enhancement with surrounding peripancreatic free fluid without evidence of pancreatic necrosis. She was intubated, started on intravenous (IV) fluids, broad-spectrum antibiotics and admitted into the Intensive Care Unit with the clinical impression of severe pancreatitis complicated with acute respiratory distress syndrome. After extubation, the patient reported a two-month onset of recurrent fevers, arthralgias, and facial rash. Serology was remarkable for normal serum IgG4 levels, positive antinuclear antibodies and hypocomplementemia. Despite receiving IV fluids and nothing by mouth, her clinical condition deteriorated, prompting the use of IV methylprednisolone. The patient continued treatment with steroids, hydroxychloroquine, and cyclophosphamide. Eventually, the patient was transitioned to oral prednisone and discharged with outpatient follow-up care.
Discussion: Although uncommon, this case highlights the significance of contemplating acute pancreatitis as a potential consequence of SLE. The rapid and appropriate medical intervention with corticosteroids played a critical role especially in individuals without a known medical history of autoimmune diseases. Ultimately, this case serves as a reminder of the need for a high index of suspicion and a comprehensive diagnostic approach when confronted with unusual clinical presentations.

Disclosures:
José M.. Bretón, MD, José M. Hernández, MD, Paola N. Laracuente, MD, Tania M. Aguila, MD, Mark A. Vergara, MD. P1810 - The Ultimate Run: Acute Pancreatitis as the Debut of Systemic Lupus Erythematosus (SLE), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
Introduction: SLE is an autoimmune disease that affects multiple organ systems. The majority of patients will debut with musculoskeletal and dermatological manifestations. However, the gastrointestinal system is less likely to be involved, with symptoms occurring in half of cases. Occasionally, pancreatitis can occur as a rare complication, with an incidence rate of up to 8.2%. Typically, it manifests as widespread flare-ups in individuals already diagnosed, making its occurrence as the initial presentation exceedingly unusual. In fact, only limited number of cases have been documented in the literature where pancreatitis precedes SLE diagnosis.
Case Description/Methods: A 36-year-old female athlete presented with hypoactivity and altered mental status. Upon evaluation, she was hypotensive, tachycardic and encephalopathic. Physical exam revealed a distended abdomen associated with epigastric, and left lower quadrant pain on deep tenderness without rebound. Laboratories revealed neutrophilia, bandemia, anemia, hypoalbuminemia, hypocalcemia, negative toxicology, normal triglycerides, and elevated inflammatory markers, amylase, and lipase. Imaging studies showed a homogenous enhancement with surrounding peripancreatic free fluid without evidence of pancreatic necrosis. She was intubated, started on intravenous (IV) fluids, broad-spectrum antibiotics and admitted into the Intensive Care Unit with the clinical impression of severe pancreatitis complicated with acute respiratory distress syndrome. After extubation, the patient reported a two-month onset of recurrent fevers, arthralgias, and facial rash. Serology was remarkable for normal serum IgG4 levels, positive antinuclear antibodies and hypocomplementemia. Despite receiving IV fluids and nothing by mouth, her clinical condition deteriorated, prompting the use of IV methylprednisolone. The patient continued treatment with steroids, hydroxychloroquine, and cyclophosphamide. Eventually, the patient was transitioned to oral prednisone and discharged with outpatient follow-up care.
Discussion: Although uncommon, this case highlights the significance of contemplating acute pancreatitis as a potential consequence of SLE. The rapid and appropriate medical intervention with corticosteroids played a critical role especially in individuals without a known medical history of autoimmune diseases. Ultimately, this case serves as a reminder of the need for a high index of suspicion and a comprehensive diagnostic approach when confronted with unusual clinical presentations.

Figure: Abdominopelvic computerized tomography scan with IV contrast showed a homogenous enhancement with surrounding peripancreatic free fluid without evidence of necrosis associated with diffuse mesenteric edema.
Disclosures:
José Bretón indicated no relevant financial relationships.
José Hernández indicated no relevant financial relationships.
Paola Laracuente indicated no relevant financial relationships.
Tania Aguila indicated no relevant financial relationships.
Mark Vergara indicated no relevant financial relationships.
José M.. Bretón, MD, José M. Hernández, MD, Paola N. Laracuente, MD, Tania M. Aguila, MD, Mark A. Vergara, MD. P1810 - The Ultimate Run: Acute Pancreatitis as the Debut of Systemic Lupus Erythematosus (SLE), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
