Monday Poster Session
Category: Biliary/Pancreas
P1812 - Benign Recurrent Intrahepatic Cholestasis Misdiagnosed as Progressive Familial Intrahepatic Cholestasis in Childhood: A Rare Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Stephanie Mrowczynski, MD
Tulane School of Medicine
New Orleans, LA
Presenting Author(s)
Stephanie Mrowczynski, MD, Jason Mathias, MD, Molly Delk, MD
Tulane School of Medicine, New Orleans, LA
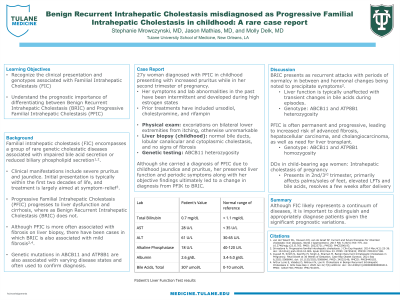
Introduction: Familial intrahepatic cholestasis (FIC) encompasses a group of rare genetic cholestatic diseases associated with impaired bile acid secretion or reduced biliary phospholipid secretion1,2. The most common clinical manifestations include severe pruritus and jaundice. Initial presentation is typically within the first two decades of life and treatment is largely aimed at symptom-relief3. An important distinguishing factor between two phenotypes, Progressive Familial Intrahepatic Cholestasis (PFIC) and Benign Recurrent Intrahepatic Cholestasis (BRIC), is progression to liver dysfunction and cirrhosis in PFIC, versus the lack of progression in BRIC. Genetic mutations in ABCB11 and ATP8B1 are also associated with varying disease states and often used to confirm diagnosis.
Case Description/Methods: We present this case of a 27y woman diagnosed with PFIC in childhood presenting with increased pruritus while in her second trimester of pregnancy. Her symptoms and lab abnormalities in the past have been intermittent and developed during high estrogen states. She has elevated alkaline phosphatase and bile acids, though the remainder of her liver chemistries are normal. Prior treatments have included ursodiol, cholestyramine, and rifampin. Physical exam is pertinent for excoriations on both lower extremities but otherwise unremarkable. Review of childhood records reveals a liver biopsy with normal bile ducts, lobular canalicular and cytoplasmic cholestasis, and no signs of fibrosis. Genetic testing reveals ABCB11 heterozygosity. Although she carried a diagnosis of PFIC due to childhood jaundice and pruritus, her preserved liver function and periodic symptoms along with her objective findings ultimately led to a change in diagnosis from PFIK to BRIC.
Discussion: BRIC presents as recurrent attacks with periods of normalcy in between and hormonal changes being noted to precipitate symptoms2. Liver function is typically unaffected with transient changes in bile acids during episodes. This is in contrast to PFIC which is often permanent and progressive, leading to increased risk of advanced fibrosis, hepatocellular carcinoma, and cholangiocarcinoma, as well as need for liver transplant. Although PFIC is more often associated with fibrosis on liver biopsy, there have been cases in which BRIC is also associated with mild fibrosis2,4. Ultimately, the gold standard for diagnosis is genetic testing for mutations in ABCB11 and ATP8B1, with heterozygosity more indicative of BRIC and homozygosity more indicative of PFIC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Stephanie Mrowczynski, MD, Jason Mathias, MD, Molly Delk, MD. P1812 - Benign Recurrent Intrahepatic Cholestasis Misdiagnosed as Progressive Familial Intrahepatic Cholestasis in Childhood: A Rare Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Tulane School of Medicine, New Orleans, LA
Introduction: Familial intrahepatic cholestasis (FIC) encompasses a group of rare genetic cholestatic diseases associated with impaired bile acid secretion or reduced biliary phospholipid secretion1,2. The most common clinical manifestations include severe pruritus and jaundice. Initial presentation is typically within the first two decades of life and treatment is largely aimed at symptom-relief3. An important distinguishing factor between two phenotypes, Progressive Familial Intrahepatic Cholestasis (PFIC) and Benign Recurrent Intrahepatic Cholestasis (BRIC), is progression to liver dysfunction and cirrhosis in PFIC, versus the lack of progression in BRIC. Genetic mutations in ABCB11 and ATP8B1 are also associated with varying disease states and often used to confirm diagnosis.
Case Description/Methods: We present this case of a 27y woman diagnosed with PFIC in childhood presenting with increased pruritus while in her second trimester of pregnancy. Her symptoms and lab abnormalities in the past have been intermittent and developed during high estrogen states. She has elevated alkaline phosphatase and bile acids, though the remainder of her liver chemistries are normal. Prior treatments have included ursodiol, cholestyramine, and rifampin. Physical exam is pertinent for excoriations on both lower extremities but otherwise unremarkable. Review of childhood records reveals a liver biopsy with normal bile ducts, lobular canalicular and cytoplasmic cholestasis, and no signs of fibrosis. Genetic testing reveals ABCB11 heterozygosity. Although she carried a diagnosis of PFIC due to childhood jaundice and pruritus, her preserved liver function and periodic symptoms along with her objective findings ultimately led to a change in diagnosis from PFIK to BRIC.
Discussion: BRIC presents as recurrent attacks with periods of normalcy in between and hormonal changes being noted to precipitate symptoms2. Liver function is typically unaffected with transient changes in bile acids during episodes. This is in contrast to PFIC which is often permanent and progressive, leading to increased risk of advanced fibrosis, hepatocellular carcinoma, and cholangiocarcinoma, as well as need for liver transplant. Although PFIC is more often associated with fibrosis on liver biopsy, there have been cases in which BRIC is also associated with mild fibrosis2,4. Ultimately, the gold standard for diagnosis is genetic testing for mutations in ABCB11 and ATP8B1, with heterozygosity more indicative of BRIC and homozygosity more indicative of PFIC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Stephanie Mrowczynski indicated no relevant financial relationships.
Jason Mathias indicated no relevant financial relationships.
Molly Delk indicated no relevant financial relationships.
Stephanie Mrowczynski, MD, Jason Mathias, MD, Molly Delk, MD. P1812 - Benign Recurrent Intrahepatic Cholestasis Misdiagnosed as Progressive Familial Intrahepatic Cholestasis in Childhood: A Rare Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

