Monday Poster Session
Category: Biliary/Pancreas
P1813 - Catamenial Pancreatitis: A Rare Manifestation of Hereditary Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jacob Seils, DO
North Mississippi Medical Center
Tupelo, MS
Presenting Author(s)
Jacob Seils, DO1, Sumair Ozair, DO1, John Phillips, MD, PhD, FACG2, Stephen Amann, MD, FACG2
1North Mississippi Medical Center, Tupelo, MS; 2Digestive Health Specialists, P.A. - One GI, Tupelo, MS
Introduction: Hereditary pancreatitis (HP) is a rare cause of chronic pancreatitis manifesting as recurrent attacks of pancreatitis often beginning at a young age. Several genes are associated with HP including: PRSS1, SPINK1, and CFTR. A number of cofactors can influence the manifestation of clinical pancreatitis in these patients.
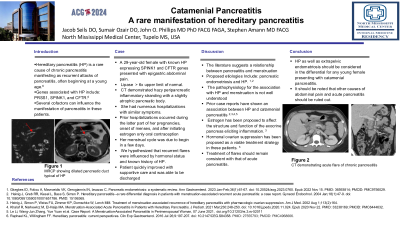
Case Description/Methods: A 29-year-old female with known HP expressing SPINK1 and CFTR genes presented to the emergency department with complaints of epigastric abdominal pain. Lipase levels were greater than 6x upper limit of normal. CT abdomen/pelvis demonstrated hazy peripancreatic inflammatory stranding with a slightly atrophic pancreatic body. The patient was diagnosed with an acute flare of chronic pancreatitis and began treatment with intravenous fluids. She had numerous hospitalizations with similar symptoms. Other mitigating factors such as hyperlipidemia, alcohol, and biliary abnormalities were not clinically pertinent. On historical analysis we found her prior hospitalizations for AP occurred during the latter part of her pregnancies, onset of her menses, and after initiating estrogen only oral contraception therapy. On this episode, her menstrual cycle was due to begin in a few days. We hypothesized that her recurrent flares of chronic pancreatitis were influenced by her hormonal status and known history of HP. After fluid resuscitation and supportive care, she clinically improved and discharged for outpatient follow-up.
Discussion: The literature suggests a relationship between pancreatitis and menstruation and is divided into to be two broad categories: pancreatic endometriosis and hereditary pancreatitis. The pathophysiology for the association with HP and menstruation is not well understood, however numerous previous case reports have shown an association. Estrogen has been proposed to affect the structure and function of the exocrine pancreas eliciting inflammation. Hormonal ovarian suppression has been proposed as a viable treatment strategy in these patients. For acute flares, treatment should remain consistent with that of AP.
HP should be considered in the differential for young female presenting with catamenial pancreatitis. It should be noted that other causes of abdominal pain and AP should be ruled out.
Disclosures:
Jacob Seils, DO1, Sumair Ozair, DO1, John Phillips, MD, PhD, FACG2, Stephen Amann, MD, FACG2. P1813 - Catamenial Pancreatitis: A Rare Manifestation of Hereditary Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1North Mississippi Medical Center, Tupelo, MS; 2Digestive Health Specialists, P.A. - One GI, Tupelo, MS
Introduction: Hereditary pancreatitis (HP) is a rare cause of chronic pancreatitis manifesting as recurrent attacks of pancreatitis often beginning at a young age. Several genes are associated with HP including: PRSS1, SPINK1, and CFTR. A number of cofactors can influence the manifestation of clinical pancreatitis in these patients.
Case Description/Methods: A 29-year-old female with known HP expressing SPINK1 and CFTR genes presented to the emergency department with complaints of epigastric abdominal pain. Lipase levels were greater than 6x upper limit of normal. CT abdomen/pelvis demonstrated hazy peripancreatic inflammatory stranding with a slightly atrophic pancreatic body. The patient was diagnosed with an acute flare of chronic pancreatitis and began treatment with intravenous fluids. She had numerous hospitalizations with similar symptoms. Other mitigating factors such as hyperlipidemia, alcohol, and biliary abnormalities were not clinically pertinent. On historical analysis we found her prior hospitalizations for AP occurred during the latter part of her pregnancies, onset of her menses, and after initiating estrogen only oral contraception therapy. On this episode, her menstrual cycle was due to begin in a few days. We hypothesized that her recurrent flares of chronic pancreatitis were influenced by her hormonal status and known history of HP. After fluid resuscitation and supportive care, she clinically improved and discharged for outpatient follow-up.
Discussion: The literature suggests a relationship between pancreatitis and menstruation and is divided into to be two broad categories: pancreatic endometriosis and hereditary pancreatitis. The pathophysiology for the association with HP and menstruation is not well understood, however numerous previous case reports have shown an association. Estrogen has been proposed to affect the structure and function of the exocrine pancreas eliciting inflammation. Hormonal ovarian suppression has been proposed as a viable treatment strategy in these patients. For acute flares, treatment should remain consistent with that of AP.
HP should be considered in the differential for young female presenting with catamenial pancreatitis. It should be noted that other causes of abdominal pain and AP should be ruled out.
Disclosures:
Jacob Seils indicated no relevant financial relationships.
Sumair Ozair indicated no relevant financial relationships.
John Phillips: AbbVie – Speakers Bureau. Gilead – Speakers Bureau. Madrigal – Speakers Bureau.
Stephen Amann indicated no relevant financial relationships.
Jacob Seils, DO1, Sumair Ozair, DO1, John Phillips, MD, PhD, FACG2, Stephen Amann, MD, FACG2. P1813 - Catamenial Pancreatitis: A Rare Manifestation of Hereditary Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
