Monday Poster Session
Category: Biliary/Pancreas
P1819 - A Bloody Gallbladder: A Case of Hemorrhagic Cholecystitis While on Dual Antiplatelet Therapy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- EH
Ermal Hasalliu, DO
Ascension Macomb-Oakland Hospital
Warren, MI
Presenting Author(s)
Ermal Hasalliu, DO1, Kaiser Kabir, DO, MS2, Shamaiza Waqas, MD2, Stephen Kehres, DO2
1Ascension Macomb-Oakland Hospital, Warren, MI; 2Ascension Macomb-Oakland Hospital, Detroit, MI
Introduction: Hemorrhagic cholecystitis (HC) is a rare condition where the gallbladder bleeds from within, often associated with increased mortality. Over 50% of cases stem from biliary obstruction by gallstones. This is a case of a patient on dual antiplatelet therapy (DAPT) who became hemodynamically unstable during hospitalization for osteomyelitis and was found to have hemorrhagic cholecystitis, which was successfully managed.
Case Description/Methods: A 65-year old male with history of heart failure, diabetes mellitus and coronary artery disease status post stent placement 8 months prior, on aspirin and clopidogrel, who originally presented for recurrent osteomyelitis. Initially, the patient was septic but improved clinically after a left 2nd digit amputation. Prior to discharge, he reported dizziness and was found to be hypotensive with a MAP < 60. There was a drop in hemoglobin from 7.0 to 5.6gm/dL within hours. He denied hematemesis, hematochezia, melena and abdominal pain. Hypotension and anemia stabilized after fluid resuscitation and transfusion with two units of packed red blood cells. Hemolysis workup was negative. CT angiography revealed gallbladder distention with a calcific gallstone mixed with a heterogeneous density from intraluminal hemorrhage. Post cholecystectomy pathology confirmed acute gangrenous cholecystitis without signs of malignancy. Post-operatively, the patient made a full recovery and DAPT was restarted once hemoglobin was stable.
Discussion: Etiologies for HC include cholelithiasis, anticoagulation, renal failure, liver cirrhosis and malignancy. While exceedingly rare, HC usually presents as abdominal pain, nausea, vomiting, and fever complicated by hypotension and shock in severe cases. Considering the lack of vascular bleeding from a neoplastic source in the pathology report, the etiology of this patient’s HC was most likely due to cholelithiasis induced inflammation with mural wall erosion leading to ischemia and necrosis. He was put at an increased risk due to DAPT. This case is an unusual example that involves current discussions regarding antiplatelets’ therapeutic benefit versus its risk of gastrointestinal bleeding. The American College of Cardiology recommends DAPT for 6-12 months based on ischemic and bleeding risk factors. Per ACG guidelines, clopidogrel can be temporarily discontinued while taking aspirin for elective procedures, but emergent cholecystectomy is vital in ensuring a positive outcome in HC.

Disclosures:
Ermal Hasalliu, DO1, Kaiser Kabir, DO, MS2, Shamaiza Waqas, MD2, Stephen Kehres, DO2. P1819 - A Bloody Gallbladder: A Case of Hemorrhagic Cholecystitis While on Dual Antiplatelet Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Macomb-Oakland Hospital, Warren, MI; 2Ascension Macomb-Oakland Hospital, Detroit, MI
Introduction: Hemorrhagic cholecystitis (HC) is a rare condition where the gallbladder bleeds from within, often associated with increased mortality. Over 50% of cases stem from biliary obstruction by gallstones. This is a case of a patient on dual antiplatelet therapy (DAPT) who became hemodynamically unstable during hospitalization for osteomyelitis and was found to have hemorrhagic cholecystitis, which was successfully managed.
Case Description/Methods: A 65-year old male with history of heart failure, diabetes mellitus and coronary artery disease status post stent placement 8 months prior, on aspirin and clopidogrel, who originally presented for recurrent osteomyelitis. Initially, the patient was septic but improved clinically after a left 2nd digit amputation. Prior to discharge, he reported dizziness and was found to be hypotensive with a MAP < 60. There was a drop in hemoglobin from 7.0 to 5.6gm/dL within hours. He denied hematemesis, hematochezia, melena and abdominal pain. Hypotension and anemia stabilized after fluid resuscitation and transfusion with two units of packed red blood cells. Hemolysis workup was negative. CT angiography revealed gallbladder distention with a calcific gallstone mixed with a heterogeneous density from intraluminal hemorrhage. Post cholecystectomy pathology confirmed acute gangrenous cholecystitis without signs of malignancy. Post-operatively, the patient made a full recovery and DAPT was restarted once hemoglobin was stable.
Discussion: Etiologies for HC include cholelithiasis, anticoagulation, renal failure, liver cirrhosis and malignancy. While exceedingly rare, HC usually presents as abdominal pain, nausea, vomiting, and fever complicated by hypotension and shock in severe cases. Considering the lack of vascular bleeding from a neoplastic source in the pathology report, the etiology of this patient’s HC was most likely due to cholelithiasis induced inflammation with mural wall erosion leading to ischemia and necrosis. He was put at an increased risk due to DAPT. This case is an unusual example that involves current discussions regarding antiplatelets’ therapeutic benefit versus its risk of gastrointestinal bleeding. The American College of Cardiology recommends DAPT for 6-12 months based on ischemic and bleeding risk factors. Per ACG guidelines, clopidogrel can be temporarily discontinued while taking aspirin for elective procedures, but emergent cholecystectomy is vital in ensuring a positive outcome in HC.

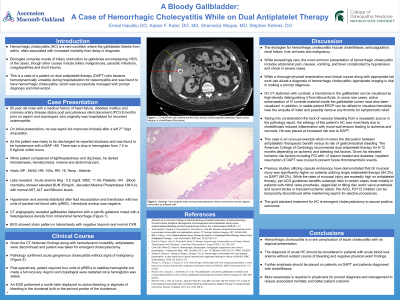
Figure: Yellow- defined borders high density contrast signifies bleeding
Red- the margins of cholelithiasis
Red- the margins of cholelithiasis
Disclosures:
Ermal Hasalliu indicated no relevant financial relationships.
Kaiser Kabir indicated no relevant financial relationships.
Shamaiza Waqas indicated no relevant financial relationships.
Stephen Kehres indicated no relevant financial relationships.
Ermal Hasalliu, DO1, Kaiser Kabir, DO, MS2, Shamaiza Waqas, MD2, Stephen Kehres, DO2. P1819 - A Bloody Gallbladder: A Case of Hemorrhagic Cholecystitis While on Dual Antiplatelet Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
