Monday Poster Session
Category: Biliary/Pancreas
P1825 - From Abdominal Pain to ICU: A Cascade of Stills Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kelvin Fernandez, MD
Newark Beth Israel Medical Center
Newark, NJ
Presenting Author(s)
Award: Presidential Poster Award
Kelvin Fernandez, MD, Allen George, MD, Syed Haider, MD, Sri Bendapudi, MD, Saamia Javed, MD
Newark Beth Israel Medical Center, Newark, NJ
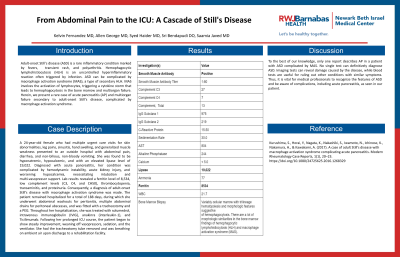
Introduction: Adult-onset Still's disease (ASD) is a rare inflammatory condition marked by fevers, transient rash, and polyarthritis. Hemophagocytic lymphohistiocytosis (HLH) is an uncontrolled hyperinflammatory reaction often triggered by infection. ASD can be complicated by macrophage activation syndrome (MAS), a type of secondary HLH. MAS involves the activation of lymphocytes, triggering a cytokine storm that leads to hemophagocytosis in the bone marrow and multiorgan failure. Herein, we present a rare case of acute pancreatitis (AP) and multiorgan failure secondary to adult-onset Still's disease, complicated by macrophage activation syndrome.
Case Description/Methods: A 24-year-old female who had multiple urgent care visits for skin abnormalities, leg pains, sinusitis, hand swelling, and generalized muscle weakness presented to an outside hospital with abdominal pain, diarrhea, and non-bilious, non-bloody vomiting. She was found to be hyponatremic, hypocalcemic, and with an elevated lipase level of 19,022. Diagnosed with acute pancreatitis, her condition was complicated by hemodynamic instability, acute kidney injury, and worsening hypocalcemia, necessitating intubation and multi-vasopressor support. Lab results revealed a ferritin level of 8,534, low complement levels (C3, C4, and CH50), thrombocytopenia, transaminitis, and proteinuria. Consequently, a diagnosis of adult-onset Still’s disease with macrophage activation syndrome was made. The patient remained hospitalized for a total of 188 days, during which she underwent abdominal washouts for peritonitis, multiple abdominal drains for peritoneal abscesses, and was fitted with a tracheostomy and a PEG. Throughout her hospitalization, she was treated with solumedrol, intravenous immunoglobulin (IVIG), anakinra (interleukin-1), and Ticilimumab. Following her prolonged ICU course, the patient began to show steady improvement, weaning off vasopressors, sedation, and the ventilator. She had the tracheostomy tube removed and was breathing on ambient air upon discharge to a rehabilitation facility.
Discussion: To the best of our knowledge, only one report describes AP in a patient with ASD complicated by MAS. No single test can definitively diagnose ASD. Imaging tests can reveal damage caused by the disease, while blood tests are useful for ruling out other conditions with similar symptoms. Thus, it is vital for medical professionals to recognize the features of ASD and be aware of complications, including acute pancreatitis, as seen in our patient.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kelvin Fernandez, MD, Allen George, MD, Syed Haider, MD, Sri Bendapudi, MD, Saamia Javed, MD. P1825 - From Abdominal Pain to ICU: A Cascade of Stills Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kelvin Fernandez, MD, Allen George, MD, Syed Haider, MD, Sri Bendapudi, MD, Saamia Javed, MD
Newark Beth Israel Medical Center, Newark, NJ
Introduction: Adult-onset Still's disease (ASD) is a rare inflammatory condition marked by fevers, transient rash, and polyarthritis. Hemophagocytic lymphohistiocytosis (HLH) is an uncontrolled hyperinflammatory reaction often triggered by infection. ASD can be complicated by macrophage activation syndrome (MAS), a type of secondary HLH. MAS involves the activation of lymphocytes, triggering a cytokine storm that leads to hemophagocytosis in the bone marrow and multiorgan failure. Herein, we present a rare case of acute pancreatitis (AP) and multiorgan failure secondary to adult-onset Still's disease, complicated by macrophage activation syndrome.
Case Description/Methods: A 24-year-old female who had multiple urgent care visits for skin abnormalities, leg pains, sinusitis, hand swelling, and generalized muscle weakness presented to an outside hospital with abdominal pain, diarrhea, and non-bilious, non-bloody vomiting. She was found to be hyponatremic, hypocalcemic, and with an elevated lipase level of 19,022. Diagnosed with acute pancreatitis, her condition was complicated by hemodynamic instability, acute kidney injury, and worsening hypocalcemia, necessitating intubation and multi-vasopressor support. Lab results revealed a ferritin level of 8,534, low complement levels (C3, C4, and CH50), thrombocytopenia, transaminitis, and proteinuria. Consequently, a diagnosis of adult-onset Still’s disease with macrophage activation syndrome was made. The patient remained hospitalized for a total of 188 days, during which she underwent abdominal washouts for peritonitis, multiple abdominal drains for peritoneal abscesses, and was fitted with a tracheostomy and a PEG. Throughout her hospitalization, she was treated with solumedrol, intravenous immunoglobulin (IVIG), anakinra (interleukin-1), and Ticilimumab. Following her prolonged ICU course, the patient began to show steady improvement, weaning off vasopressors, sedation, and the ventilator. She had the tracheostomy tube removed and was breathing on ambient air upon discharge to a rehabilitation facility.
Discussion: To the best of our knowledge, only one report describes AP in a patient with ASD complicated by MAS. No single test can definitively diagnose ASD. Imaging tests can reveal damage caused by the disease, while blood tests are useful for ruling out other conditions with similar symptoms. Thus, it is vital for medical professionals to recognize the features of ASD and be aware of complications, including acute pancreatitis, as seen in our patient.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kelvin Fernandez indicated no relevant financial relationships.
Allen George indicated no relevant financial relationships.
Syed Haider indicated no relevant financial relationships.
Sri Bendapudi indicated no relevant financial relationships.
Saamia Javed indicated no relevant financial relationships.
Kelvin Fernandez, MD, Allen George, MD, Syed Haider, MD, Sri Bendapudi, MD, Saamia Javed, MD. P1825 - From Abdominal Pain to ICU: A Cascade of Stills Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

