Monday Poster Session
Category: Biliary/Pancreas
P1830 - A Case of Chronic Pancreatitis due to Primary Hyperparathyroidism and the Barriers to Definitive Treatment
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mark DeSantis, DO, MS
AtlantiCare Regional Medical Center
Brigantine, NJ
Presenting Author(s)
Mark DeSantis, DO, MS1, Ciarra Yap, MD1, Alec Massood, DO, MS2, VonPatrick DelaRosa, MD1, Thien Hoang, DO1
1AtlantiCare Regional Medical Center, Atlantic City, NJ; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction:
One of the rare etiologies of chronic pancreatitis (CP) is hypercalcemia. Hypercalcemia is a relatively common problem in the United States with the two most common causes including primary hyperparathyroidism (PHPT) and malignancy. Hypercalcemia from PHPT can lead to CP but the prevalence is low.
Case Description/Methods:
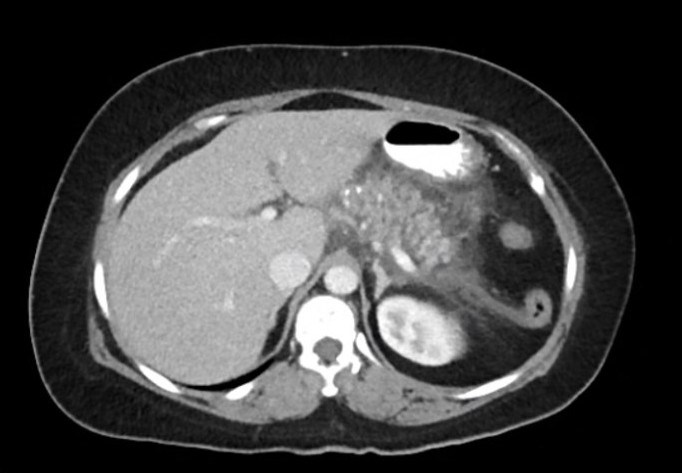
A 49 year old female with no reported past medical history presented to the hospital due to generalized abdominal pain with nausea and vomiting. She reported similar episodes every 3-4 months for the past 2-3 years without any formal medical evaluation. She recently emigrated from Bangladesh to the US. Laboratory values were significant for calcium 14.3, Alk Phos 177, Lipase 2164, Triglyceride level 97, and WBC 16.4. CTAP with contrast revealed acute on chronic pancreatitis without fluid collection. Other relevant labs were PTH 407, Vitamin D 25 7.0, phosphorus 1.7, and Urine calcium 517. Nuclear medicine scan of the parathyroid showed left upper parathyroid adenoma. She was recommended to undergo parathyroidectomy but there were no specialized surgeons at the current center. Therefore, she was recommended for outpatient evaluation at a tertiary medical center and was discharged. In the following months, she established care at the region's Federally Qualified Health Center (FQHC) where she complained of recurrent abdominal pain. After a 3 month wait for an appointment, she established care with outpatient endocrinology at the FQHC. Repeat lab work showed hypercalcemia. She was referred again to a specialized center for surgical intervention.
Discussion:
CP is an inflammatory condition that results in permanent structural changes in the pancreas leading to impairment of exocrine and endocrine function which can lead to various complications. The treatment for PHPT in select patients is parathyroidectomy. The rate of recurrent pancreatitis is generally low after parathyroidectomy. There are many barriers as to why this patient has not received parathyroidectomy including language barrier, availability of trained surgeons, insurance status, wait times for specialty care for the uninsured, and provider/patient education. At the time of this case report, she is 7 months since her initial hospitalization and has not yet undergone parathyroidectomy. Without addressing the barriers related to this patient's care, she may develop additional complications of CP which would contribute to increased morbidity and mortality.
Disclosures:
Mark DeSantis, DO, MS1, Ciarra Yap, MD1, Alec Massood, DO, MS2, VonPatrick DelaRosa, MD1, Thien Hoang, DO1. P1830 - A Case of Chronic Pancreatitis due to Primary Hyperparathyroidism and the Barriers to Definitive Treatment, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1AtlantiCare Regional Medical Center, Atlantic City, NJ; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction:
One of the rare etiologies of chronic pancreatitis (CP) is hypercalcemia. Hypercalcemia is a relatively common problem in the United States with the two most common causes including primary hyperparathyroidism (PHPT) and malignancy. Hypercalcemia from PHPT can lead to CP but the prevalence is low.
Case Description/Methods:
A 49 year old female with no reported past medical history presented to the hospital due to generalized abdominal pain with nausea and vomiting. She reported similar episodes every 3-4 months for the past 2-3 years without any formal medical evaluation. She recently emigrated from Bangladesh to the US. Laboratory values were significant for calcium 14.3, Alk Phos 177, Lipase 2164, Triglyceride level 97, and WBC 16.4. CTAP with contrast revealed acute on chronic pancreatitis without fluid collection. Other relevant labs were PTH 407, Vitamin D 25 7.0, phosphorus 1.7, and Urine calcium 517. Nuclear medicine scan of the parathyroid showed left upper parathyroid adenoma. She was recommended to undergo parathyroidectomy but there were no specialized surgeons at the current center. Therefore, she was recommended for outpatient evaluation at a tertiary medical center and was discharged. In the following months, she established care at the region's Federally Qualified Health Center (FQHC) where she complained of recurrent abdominal pain. After a 3 month wait for an appointment, she established care with outpatient endocrinology at the FQHC. Repeat lab work showed hypercalcemia. She was referred again to a specialized center for surgical intervention.
Discussion:
CP is an inflammatory condition that results in permanent structural changes in the pancreas leading to impairment of exocrine and endocrine function which can lead to various complications. The treatment for PHPT in select patients is parathyroidectomy. The rate of recurrent pancreatitis is generally low after parathyroidectomy. There are many barriers as to why this patient has not received parathyroidectomy including language barrier, availability of trained surgeons, insurance status, wait times for specialty care for the uninsured, and provider/patient education. At the time of this case report, she is 7 months since her initial hospitalization and has not yet undergone parathyroidectomy. Without addressing the barriers related to this patient's care, she may develop additional complications of CP which would contribute to increased morbidity and mortality.
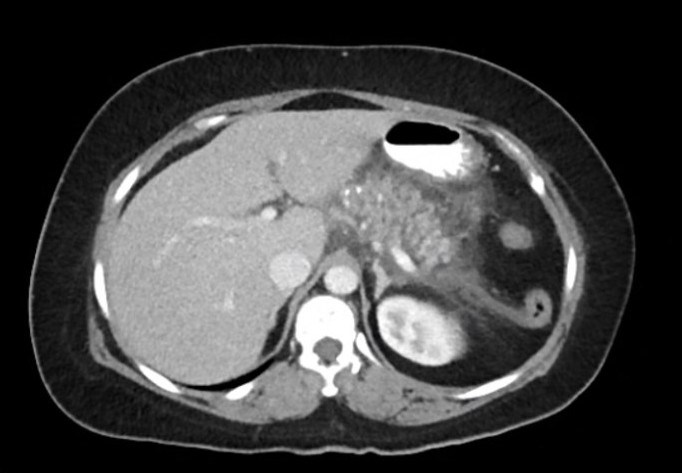
Figure: Image 1: CTAP with contrast shows acute on chronic pancreatitis
Disclosures:
Mark DeSantis indicated no relevant financial relationships.
Ciarra Yap indicated no relevant financial relationships.
Alec Massood indicated no relevant financial relationships.
VonPatrick DelaRosa indicated no relevant financial relationships.
Thien Hoang indicated no relevant financial relationships.
Mark DeSantis, DO, MS1, Ciarra Yap, MD1, Alec Massood, DO, MS2, VonPatrick DelaRosa, MD1, Thien Hoang, DO1. P1830 - A Case of Chronic Pancreatitis due to Primary Hyperparathyroidism and the Barriers to Definitive Treatment, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
