Monday Poster Session
Category: Biliary/Pancreas
P1844 - Influenza A as a Trigger of Necrotizing Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Amla A. Patel, MBBS
Creighton University
Phoenix, AZ
Presenting Author(s)
Amla A. Patel, MBBS1, Alison Russell, DO2, David Wisinger, MD3
1Creighton University, Phoenix, AZ; 2Creighton University, Scottsdale, AZ; 3Creighton University School of Medicine, Phoenix, AZ
Introduction: Acute pancreatitis is the most common cause of gastrointestinal-related hospitalization in the country with a mortality ranging from 3 to 20%. Diagnosis requires 2 of 3 criteria: abdominal pain; elevated serum lipase or amylase 3 times the upper limit of normal; and characteristic findings of pancreatitis on imaging. We discuss a patient presenting with mild acute pancreatitis progressing to necrotizing pancreatitis with Influenza A as a possible cause.
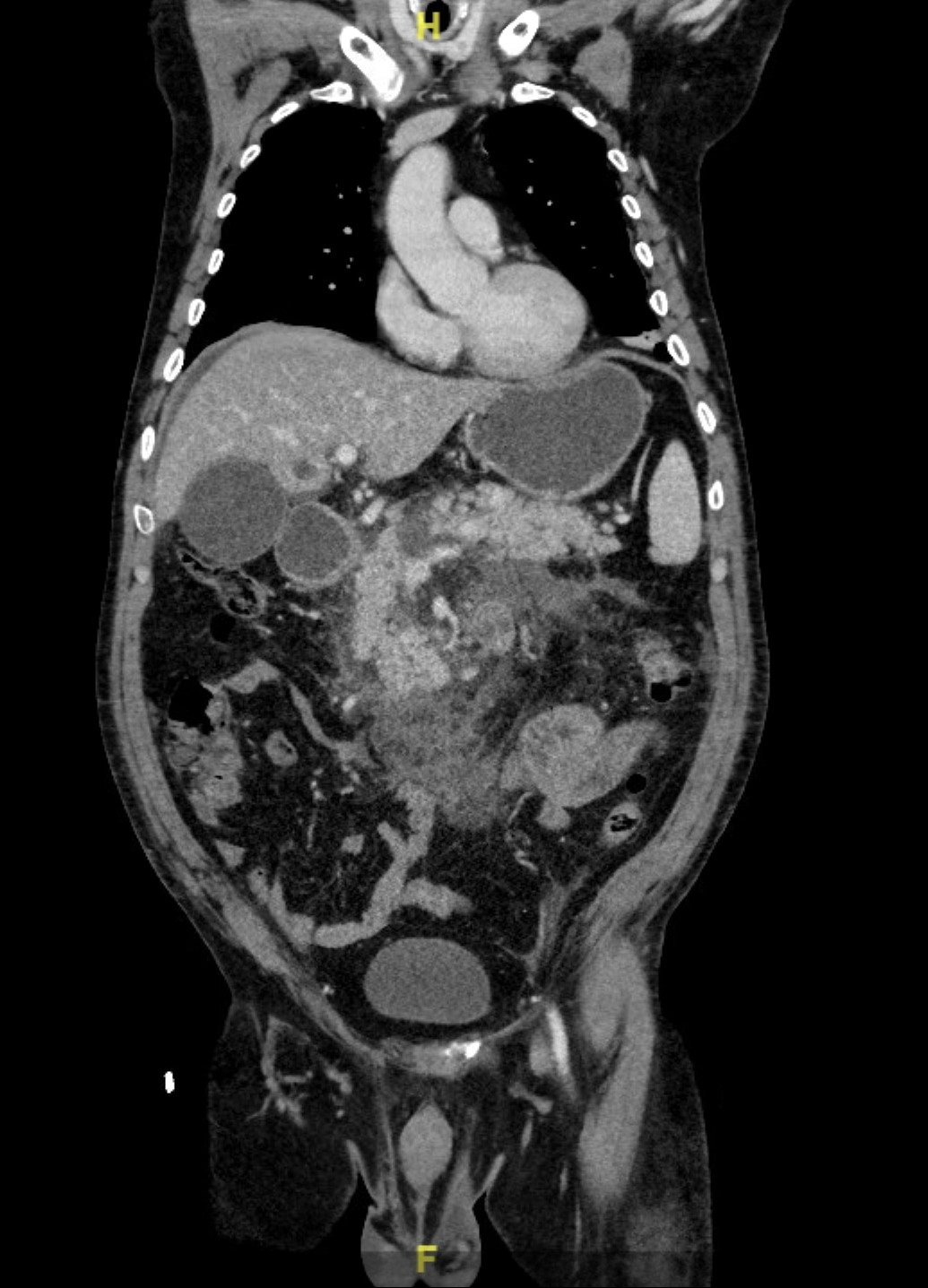
Case Description/Methods: A 62-year-old male with history of hypertension on amlodipine, rheumatoid arthritis on low dose prednisone and weekly methotrexate, presented for abdominal pain radiating to his back and vomiting for 2 days. He denied any new prescribed or OTC medications. On exam he had generalized abdominal tenderness with guarding in the epigastric region and required supplemental oxygen. Blood work showed lipase 4,731 U/L, WBC 14.4 K, and a viral swab positive for influenza A despite recent vaccination. Triglycerides were in normal range. CXR showed multilobar asymmetric infiltrates. US Abdomen ruled out cholelithiasis and CT abdomen/pelvis showed acute interstitial edematous pancreatitis without any necrosis or organizing abscess. He begun receiving supportive care along with oseltamivir however the abdominal pain worsened, and oxygen requirement increased. Procalcitonin was 0.96 ng/ml and he was started on treatment for community acquired pneumonia. A repeat CT abdomen/pelvis was done 5 days later due to worsening abdominal distention, pain, and inability to tolerate PO intake showed necrotizing pancreatitis without any increased pancreas involvement or abscess formation. He soon began tolerating PO intake with supportive care.
Discussion: Per Revised Atlanta Classification, pancreatitis severity can be split into mild acute pancreatitis with nascent organ failure, moderately severe with transient organ failure resolving in 48 hours, and severe acute with persistent organ failure involving at least one organ. In our case, the most common causes of alcohol, gallstones, hypertriglyceridemia, and medications were ruled out. Influenza A is a common virus however not typically in the differential of pancreatitis. The proposed mechanism is that the virus binds to sialic acid receptors on pancreatic cells due to tropism, inducing apoptosis and releasing pro-inflammatory cytokines. Hence Influenza A must be considered as a possible cause of pancreatitis especially during seasonal periods when other causes have been ruled out.
Disclosures:
Amla A. Patel, MBBS1, Alison Russell, DO2, David Wisinger, MD3. P1844 - Influenza A as a Trigger of Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University, Phoenix, AZ; 2Creighton University, Scottsdale, AZ; 3Creighton University School of Medicine, Phoenix, AZ
Introduction: Acute pancreatitis is the most common cause of gastrointestinal-related hospitalization in the country with a mortality ranging from 3 to 20%. Diagnosis requires 2 of 3 criteria: abdominal pain; elevated serum lipase or amylase 3 times the upper limit of normal; and characteristic findings of pancreatitis on imaging. We discuss a patient presenting with mild acute pancreatitis progressing to necrotizing pancreatitis with Influenza A as a possible cause.
Case Description/Methods: A 62-year-old male with history of hypertension on amlodipine, rheumatoid arthritis on low dose prednisone and weekly methotrexate, presented for abdominal pain radiating to his back and vomiting for 2 days. He denied any new prescribed or OTC medications. On exam he had generalized abdominal tenderness with guarding in the epigastric region and required supplemental oxygen. Blood work showed lipase 4,731 U/L, WBC 14.4 K, and a viral swab positive for influenza A despite recent vaccination. Triglycerides were in normal range. CXR showed multilobar asymmetric infiltrates. US Abdomen ruled out cholelithiasis and CT abdomen/pelvis showed acute interstitial edematous pancreatitis without any necrosis or organizing abscess. He begun receiving supportive care along with oseltamivir however the abdominal pain worsened, and oxygen requirement increased. Procalcitonin was 0.96 ng/ml and he was started on treatment for community acquired pneumonia. A repeat CT abdomen/pelvis was done 5 days later due to worsening abdominal distention, pain, and inability to tolerate PO intake showed necrotizing pancreatitis without any increased pancreas involvement or abscess formation. He soon began tolerating PO intake with supportive care.
Discussion: Per Revised Atlanta Classification, pancreatitis severity can be split into mild acute pancreatitis with nascent organ failure, moderately severe with transient organ failure resolving in 48 hours, and severe acute with persistent organ failure involving at least one organ. In our case, the most common causes of alcohol, gallstones, hypertriglyceridemia, and medications were ruled out. Influenza A is a common virus however not typically in the differential of pancreatitis. The proposed mechanism is that the virus binds to sialic acid receptors on pancreatic cells due to tropism, inducing apoptosis and releasing pro-inflammatory cytokines. Hence Influenza A must be considered as a possible cause of pancreatitis especially during seasonal periods when other causes have been ruled out.
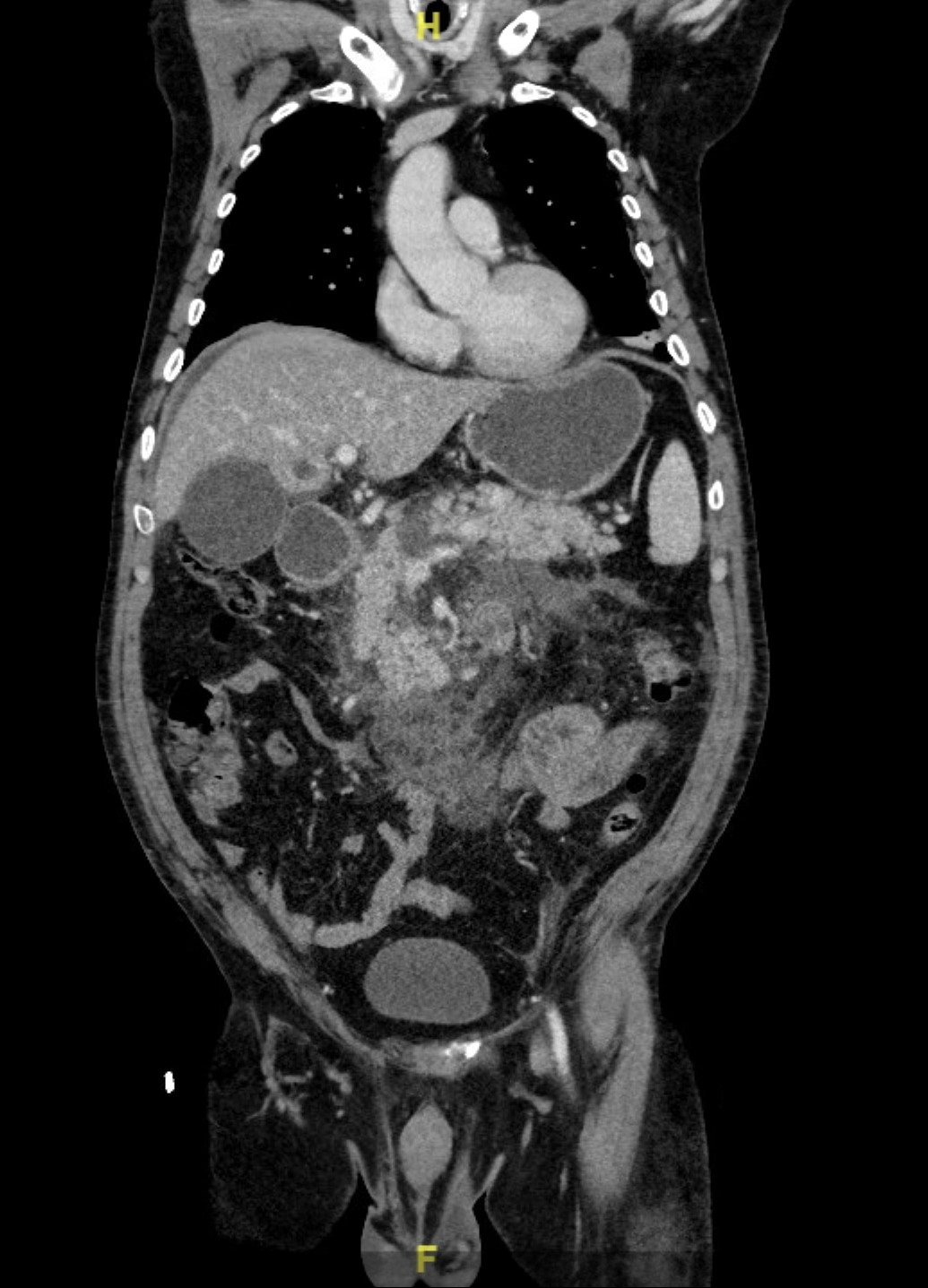
Figure: Computed tomography imaging showing necrotizing pancreatitis with peri-pancreatic fat stranding with a new area of necrosis in the pancreatic head and neck of size 1.9 cm x 2.7 cm.
Disclosures:
Amla Patel indicated no relevant financial relationships.
Alison Russell indicated no relevant financial relationships.
David Wisinger indicated no relevant financial relationships.
Amla A. Patel, MBBS1, Alison Russell, DO2, David Wisinger, MD3. P1844 - Influenza A as a Trigger of Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

