Monday Poster Session
Category: Biliary/Pancreas
P1853 - Hand, Foot, Mouth, and Pancreas? A Unique Presentation of Coxsackievirus-Induced Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shaina Ailawadi, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Shaina Ailawadi, MD, Shwetha Sudhakar, MD, Giselle Dutcher, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: While gallstones and alcohol use are the most common causes of acute pancreatitis (AP), approximately 10% of AP cases are caused by infectious microorganisms. Describing cases of AP as idiopathic may halt diagnostic work-up, leading to harm by ineffective treatment, unnecessary procedures, and worsening of the untreated infection. We present a patient with a severe and unusual presentation of Coxsackievirus pancreatitis.
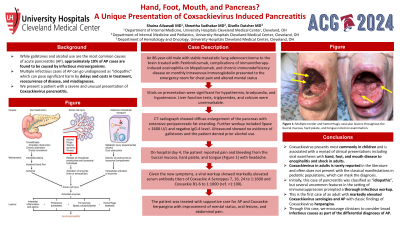
Case Description/Methods: An 86-year-old male with stable lung adenocarcinoma metastatic to the brain treated with Pembrolizumab, immunotherapy-induced eosinophilia on Mepolizumab, and chronic immunodeficiency disease on monthly intravenous immunoglobulin presented to the emergency room for chest pain and confusion. Vitals on presentation were significant for hypothermia, bradycardia, and hypotension. Liver function tests, triglycerides, and calcium were unremarkable. Serum lipase was > 2600 U/L and IgG-4 level was negative. Ultrasound showed no evidence of gallstones and the patient did not drink alcohol. CT-radiograph showed diffuse enlargement of the pancreas with extensive peripancreatic fat stranding. His home medications were not associated with AP. On hospital day 4, the patient reported pain and bleeding from the buccal mucosa, hard palate, and tongue (Figure 1) with headache. Viral workup for the new symptoms revealed markedly elevated serum antibody titers of Coxsackie A Serotypes 7, 16, 24 to 1:1600 and Coxsackie B1-6 to 1:1000 (ref. < 1:100). The patient received supportive care for Coxsackie herpangina with improvement of mental status, oral lesions, and abdominal pain.
Discussion: Coxsackievirus is well-known to pediatricians and has a myriad of clinical presentations. Children have fever, hand, foot, and mouth sores. Coxsackievirus in adults is rarely reported. Adult patients often do not present with the classic pediatric rash. Notably, our patient had mouth sores but no hand or foot lesions. The pancreatitis was classified as idiopathic and the oral lesions were initially overlooked. Headache prompted a thorough infectious workup and revealed a unifying diagnosis for AP, mouth sores, and confusion. This is the first case of an adult with markedly elevated Coxsackievirus serologies and AP with classic findings of Coxsackievirus herpangina. We encourage clinicians to consider infectious causes as part of the differential diagnosis of AP.

Disclosures:
Shaina Ailawadi, MD, Shwetha Sudhakar, MD, Giselle Dutcher, MD. P1853 - Hand, Foot, Mouth, and Pancreas? A Unique Presentation of Coxsackievirus-Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: While gallstones and alcohol use are the most common causes of acute pancreatitis (AP), approximately 10% of AP cases are caused by infectious microorganisms. Describing cases of AP as idiopathic may halt diagnostic work-up, leading to harm by ineffective treatment, unnecessary procedures, and worsening of the untreated infection. We present a patient with a severe and unusual presentation of Coxsackievirus pancreatitis.
Case Description/Methods: An 86-year-old male with stable lung adenocarcinoma metastatic to the brain treated with Pembrolizumab, immunotherapy-induced eosinophilia on Mepolizumab, and chronic immunodeficiency disease on monthly intravenous immunoglobulin presented to the emergency room for chest pain and confusion. Vitals on presentation were significant for hypothermia, bradycardia, and hypotension. Liver function tests, triglycerides, and calcium were unremarkable. Serum lipase was > 2600 U/L and IgG-4 level was negative. Ultrasound showed no evidence of gallstones and the patient did not drink alcohol. CT-radiograph showed diffuse enlargement of the pancreas with extensive peripancreatic fat stranding. His home medications were not associated with AP. On hospital day 4, the patient reported pain and bleeding from the buccal mucosa, hard palate, and tongue (Figure 1) with headache. Viral workup for the new symptoms revealed markedly elevated serum antibody titers of Coxsackie A Serotypes 7, 16, 24 to 1:1600 and Coxsackie B1-6 to 1:1000 (ref. < 1:100). The patient received supportive care for Coxsackie herpangina with improvement of mental status, oral lesions, and abdominal pain.
Discussion: Coxsackievirus is well-known to pediatricians and has a myriad of clinical presentations. Children have fever, hand, foot, and mouth sores. Coxsackievirus in adults is rarely reported. Adult patients often do not present with the classic pediatric rash. Notably, our patient had mouth sores but no hand or foot lesions. The pancreatitis was classified as idiopathic and the oral lesions were initially overlooked. Headache prompted a thorough infectious workup and revealed a unifying diagnosis for AP, mouth sores, and confusion. This is the first case of an adult with markedly elevated Coxsackievirus serologies and AP with classic findings of Coxsackievirus herpangina. We encourage clinicians to consider infectious causes as part of the differential diagnosis of AP.

Figure: Figure 1: Multiple tender and hemorrhagic vesicular lesions throughout the buccal mucosa, hard palate, and tongue noted on examination.
Disclosures:
Shaina Ailawadi indicated no relevant financial relationships.
Shwetha Sudhakar indicated no relevant financial relationships.
Giselle Dutcher indicated no relevant financial relationships.
Shaina Ailawadi, MD, Shwetha Sudhakar, MD, Giselle Dutcher, MD. P1853 - Hand, Foot, Mouth, and Pancreas? A Unique Presentation of Coxsackievirus-Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

