Monday Poster Session
Category: Biliary/Pancreas
P1854 - Undiagnosed Sarcoidosis Presenting as Hypercalcemia-Induced Acute Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SN
Stephany Nguyen, MD
LSU
New Orleans, LA
Presenting Author(s)
Stephany Nguyen, MD, John F. G.. Bobo, MD, Allison Pinner, MD, Edward Leonard, MD
LSU, New Orleans, LA
Introduction: Almost half of the cases of sarcoidosis are incidentally diagnosed after lung imaging is obtained for an unrelated reason. However, it is important to keep in mind that sarcoidosis can have extrapulmonary manifestations, which this case aims to discuss.
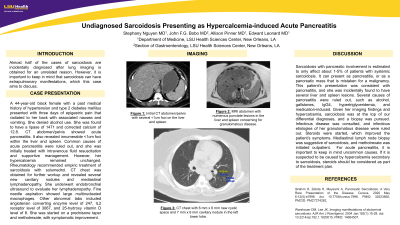
Case Description/Methods: A 44-year-old black female with a past medical history of hypertension and type 2 diabetes mellitus presented with three days of epigastric pain that radiated to her back with associated nausea and vomiting. She denied alcohol use. She was found to have a lipase of 1471 and corrected calcium of 12.8. CT abdomen/pelvis showed acute pancreatitis. It also revealed innumerable < 1cm foci within the liver and spleen. Common causes of acute pancreatitis were ruled out, and she was initially treated with intravenous fluid resuscitation and supportive management. However, her hypercalcemia remained unchanged. Rheumatology recommended empiric treatment of sarcoidosis with solumedrol. CT chest was obtained for further workup and revealed several new cavitary nodules and mediastinal lymphadenopathy. She underwent endobronchial ultrasound to evaluate her lymphadenopathy. Fine needle aspiration showed large multinucleated macrophages. Other abnormal labs included angiotensin converting enzyme level of 247, IL2 receptor level of 3067, and 25-hydroxy vitamin D level of 8. She was started on a prednisone taper and methotrexate, with symptomatic improvement.
Discussion: Sarcoidosis with pancreatic involvement is estimated to only affect about 1-5% of patients with systemic sarcoidosis. It can present as pancreatitis, or as a pancreatic mass that is mistaken for a malignancy. This patient’s presentation was consistent with pancreatitis, and she was incidentally found to have several liver and spleen lesions. Several causes of pancreatitis were ruled out, such as alcohol, gallstones, IgG4, hypertriglyceridemia, and medication-induced. Given her imaging findings and hypercalcemia, sarcoidosis was at the top of our differential diagnoses, and a biopsy was pursued. Infectious disease was consulted, and infectious etiologies of her granulomatous disease were ruled out. Steroids were started, which improved the patient’s symptoms. Mediastinal lymph node biopsy was suggestive of sarcoidosis, and methotrexate was initiated outpatient. For acute pancreatitis, it is important to keep in mind uncommon causes. If it is suspected to be caused by hypercalcemia secondary to sarcoidosis, steroids should be considered as part of the treatment plan.
Disclosures:
Stephany Nguyen, MD, John F. G.. Bobo, MD, Allison Pinner, MD, Edward Leonard, MD. P1854 - Undiagnosed Sarcoidosis Presenting as Hypercalcemia-Induced Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
LSU, New Orleans, LA
Introduction: Almost half of the cases of sarcoidosis are incidentally diagnosed after lung imaging is obtained for an unrelated reason. However, it is important to keep in mind that sarcoidosis can have extrapulmonary manifestations, which this case aims to discuss.
Case Description/Methods: A 44-year-old black female with a past medical history of hypertension and type 2 diabetes mellitus presented with three days of epigastric pain that radiated to her back with associated nausea and vomiting. She denied alcohol use. She was found to have a lipase of 1471 and corrected calcium of 12.8. CT abdomen/pelvis showed acute pancreatitis. It also revealed innumerable < 1cm foci within the liver and spleen. Common causes of acute pancreatitis were ruled out, and she was initially treated with intravenous fluid resuscitation and supportive management. However, her hypercalcemia remained unchanged. Rheumatology recommended empiric treatment of sarcoidosis with solumedrol. CT chest was obtained for further workup and revealed several new cavitary nodules and mediastinal lymphadenopathy. She underwent endobronchial ultrasound to evaluate her lymphadenopathy. Fine needle aspiration showed large multinucleated macrophages. Other abnormal labs included angiotensin converting enzyme level of 247, IL2 receptor level of 3067, and 25-hydroxy vitamin D level of 8. She was started on a prednisone taper and methotrexate, with symptomatic improvement.
Discussion: Sarcoidosis with pancreatic involvement is estimated to only affect about 1-5% of patients with systemic sarcoidosis. It can present as pancreatitis, or as a pancreatic mass that is mistaken for a malignancy. This patient’s presentation was consistent with pancreatitis, and she was incidentally found to have several liver and spleen lesions. Several causes of pancreatitis were ruled out, such as alcohol, gallstones, IgG4, hypertriglyceridemia, and medication-induced. Given her imaging findings and hypercalcemia, sarcoidosis was at the top of our differential diagnoses, and a biopsy was pursued. Infectious disease was consulted, and infectious etiologies of her granulomatous disease were ruled out. Steroids were started, which improved the patient’s symptoms. Mediastinal lymph node biopsy was suggestive of sarcoidosis, and methotrexate was initiated outpatient. For acute pancreatitis, it is important to keep in mind uncommon causes. If it is suspected to be caused by hypercalcemia secondary to sarcoidosis, steroids should be considered as part of the treatment plan.
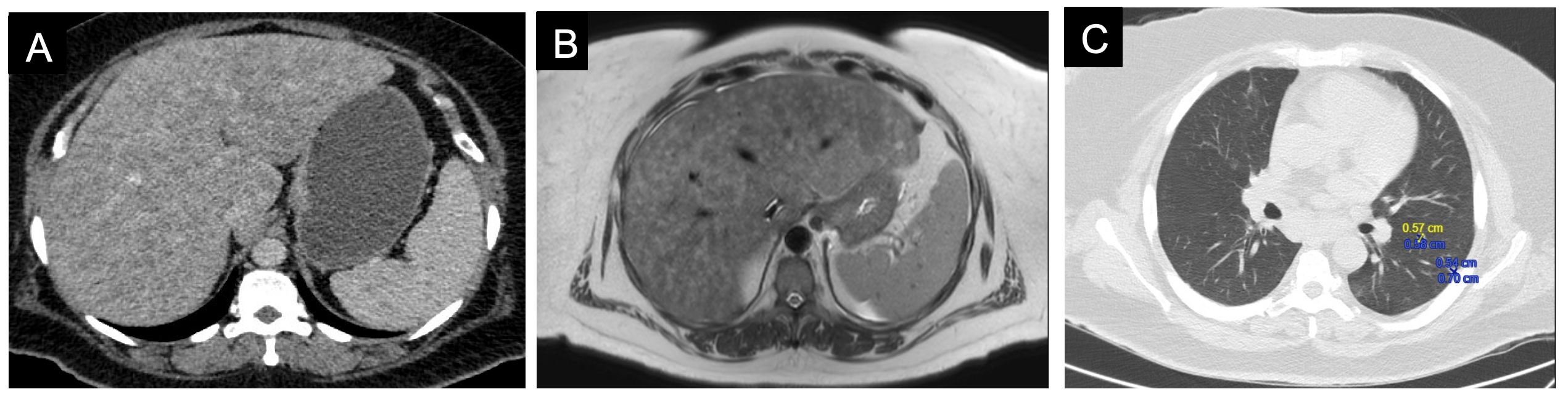
Figure: Figure A: Initial CT abdomen/pelvis with several <1cm foci on the liver and spleen.
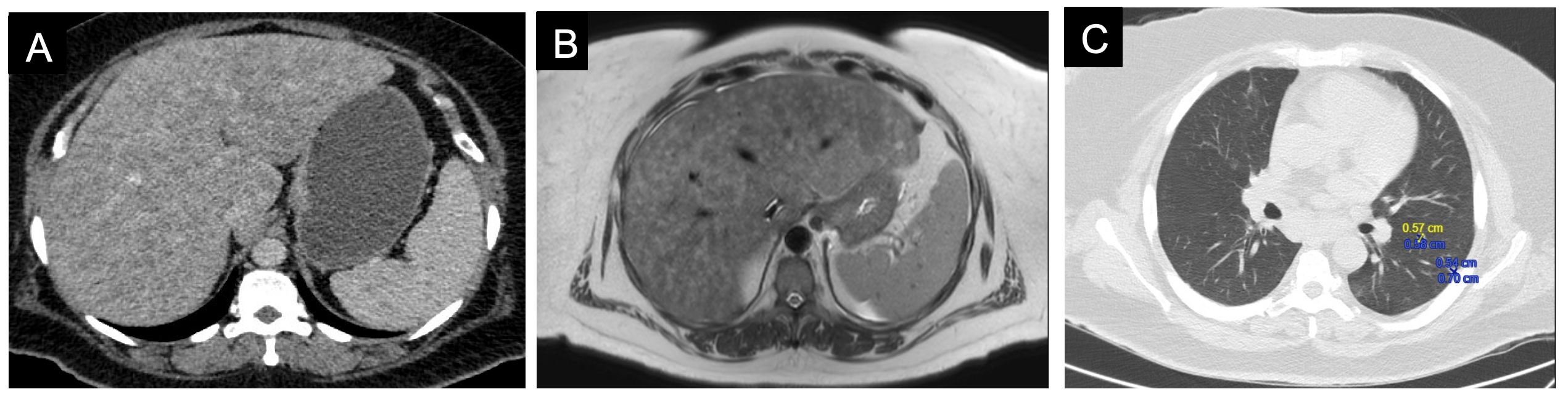
Figure B: MRI abdomen with numerous punctate lesions in the liver and spleen concerning for granulomatous disease.
Figure C: CT chest with 6 mm x 6 mm new cystic space and 7 mm x 6 mm cavitary nodule in the left lower lobe.
Figure B: MRI abdomen with numerous punctate lesions in the liver and spleen concerning for granulomatous disease.
Figure C: CT chest with 6 mm x 6 mm new cystic space and 7 mm x 6 mm cavitary nodule in the left lower lobe.
Disclosures:
Stephany Nguyen indicated no relevant financial relationships.
John Bobo indicated no relevant financial relationships.
Allison Pinner indicated no relevant financial relationships.
Edward Leonard indicated no relevant financial relationships.
Stephany Nguyen, MD, John F. G.. Bobo, MD, Allison Pinner, MD, Edward Leonard, MD. P1854 - Undiagnosed Sarcoidosis Presenting as Hypercalcemia-Induced Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
