Monday Poster Session
Category: Biliary/Pancreas
P1855 - From Back Pain to Pancreatitis: An Unexpected Consequence of Epidural Steroids
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JG
Jacob Gries, MD, MSc
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Jacob Gries, MD, MSc1, Bing Chen, MD2, Kamille A. Parungao, DO3, Irene Mbih, MD3
1Geisinger Medical Center, Danville, PA; 2Geisenger Medical Center, Danville, PA; 3Geisinger Health System, Danville, PA
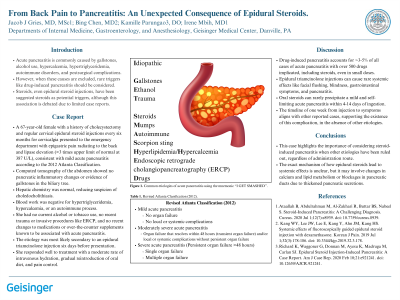
Introduction: Acute pancreatitis is commonly caused by gallstones, alcohol use, hypercalcemia, hypertriglyceridemia, autoimmune disorders, and postsurgical complications. However, when these causes are excluded, rare triggers like drug-induced pancreatitis should be considered. Steroids, even epidural steroid injections, have been suggested as a potential trigger, although this association is debated due to limited case reports or small retrospective studies.
Case Description/Methods: A 67-year-old female with a history of cholecystectomy and regular cervical epidural steroid injections every six months for cervicalgia presented to the emergency department with epigastric pain radiating to the back and lipase elevation ( >3 times upper limit of normal at 387 U/L), consistent with mild acute pancreatitis according to the 2012 Atlanta Classification. Computed tomography of the abdomen showed no pancreatic inflammatory changes or evidence of gallstones in the biliary tree. Hepatic chemistry was normal, reducing suspicion of choledocholithiasis. Blood work was negative for hypertriglyceridemia, hypercalcemia, or an autoimmune process. She had no current alcohol or tobacco use, no recent trauma or invasive procedures like ERCP, and no recent changes to medications or over-the-counter supplements known to be associated with acute pancreatitis. The etiology was most likely secondary to an epidural triamcinolone injection six days before presentation. She responded well to treatment with a moderate rate of intravenous hydration, gradual reintroduction of oral diet, and pain control.
Discussion: Epidural triamcinolone injections can cause rare systemic effects like facial flushing, blindness, gastrointestinal symptoms, and pancreatitis. This case highlights the importance of considering steroid-induced pancreatitis when other etiologies have been ruled out, regardless of administration route. The exact mechanism of how epidural steroids lead to systemic effects is unclear, but it may involve changes in calcium and lipid metabolism or blockages in pancreatic ducts due to thickened pancreatic secretions. The timeline of one week from injection to symptoms aligns with other reported cases, supporting the existence of this complication.
Disclosures:
Jacob Gries, MD, MSc1, Bing Chen, MD2, Kamille A. Parungao, DO3, Irene Mbih, MD3. P1855 - From Back Pain to Pancreatitis: An Unexpected Consequence of Epidural Steroids, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisenger Medical Center, Danville, PA; 3Geisinger Health System, Danville, PA
Introduction: Acute pancreatitis is commonly caused by gallstones, alcohol use, hypercalcemia, hypertriglyceridemia, autoimmune disorders, and postsurgical complications. However, when these causes are excluded, rare triggers like drug-induced pancreatitis should be considered. Steroids, even epidural steroid injections, have been suggested as a potential trigger, although this association is debated due to limited case reports or small retrospective studies.
Case Description/Methods: A 67-year-old female with a history of cholecystectomy and regular cervical epidural steroid injections every six months for cervicalgia presented to the emergency department with epigastric pain radiating to the back and lipase elevation ( >3 times upper limit of normal at 387 U/L), consistent with mild acute pancreatitis according to the 2012 Atlanta Classification. Computed tomography of the abdomen showed no pancreatic inflammatory changes or evidence of gallstones in the biliary tree. Hepatic chemistry was normal, reducing suspicion of choledocholithiasis. Blood work was negative for hypertriglyceridemia, hypercalcemia, or an autoimmune process. She had no current alcohol or tobacco use, no recent trauma or invasive procedures like ERCP, and no recent changes to medications or over-the-counter supplements known to be associated with acute pancreatitis. The etiology was most likely secondary to an epidural triamcinolone injection six days before presentation. She responded well to treatment with a moderate rate of intravenous hydration, gradual reintroduction of oral diet, and pain control.
Discussion: Epidural triamcinolone injections can cause rare systemic effects like facial flushing, blindness, gastrointestinal symptoms, and pancreatitis. This case highlights the importance of considering steroid-induced pancreatitis when other etiologies have been ruled out, regardless of administration route. The exact mechanism of how epidural steroids lead to systemic effects is unclear, but it may involve changes in calcium and lipid metabolism or blockages in pancreatic ducts due to thickened pancreatic secretions. The timeline of one week from injection to symptoms aligns with other reported cases, supporting the existence of this complication.
Disclosures:
Jacob Gries indicated no relevant financial relationships.
Bing Chen indicated no relevant financial relationships.
Kamille Parungao indicated no relevant financial relationships.
Irene Mbih indicated no relevant financial relationships.
Jacob Gries, MD, MSc1, Bing Chen, MD2, Kamille A. Parungao, DO3, Irene Mbih, MD3. P1855 - From Back Pain to Pancreatitis: An Unexpected Consequence of Epidural Steroids, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
