Monday Poster Session
Category: Biliary/Pancreas
P1899 - Choleperitoneum: When Your Intrahepatic Bile Duct Springs a Leak
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MB
Mehak Bassi, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Mehak Bassi, MD1, Archit Garg, MD2, Fadi Barkho, MD2, Sugirdhana Velpari, MD1, Andrew Korman, MD3
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ
Introduction: Perforation of the common bile duct after cholecystectomy is a rare and potentially fatal cause of acute abdomen, usually presenting as biliary peritonitis. Post-cholecystectomy choleperitoneum (biliary peritonitis) significantly increases the risk of postoperative mortality. We present a case report of a 45-year-old woman who developed choleperitoneum following an otherwise uneventful cholecystectomy, highlighting the importance of prompt diagnosis and management.
Case Description/Methods: A 45-year-old female presented with one-day onset of epigastric pain, nausea, and vomiting to the emergency. Imaging revealed acute pancreatitis and cholelithiasis. She underwent a robotic-assisted cholecystectomy and was discharged two days later.
She returned a week later with worsening abdominal pain and distension. Imaging indicated severe ascites and post-cholecystectomy changes. CT indicated collection at the gallbladder fossa. A hepatobiliary iminodiacetic acid scan confirmed a bile leak, indicating perforation of the bile duct.
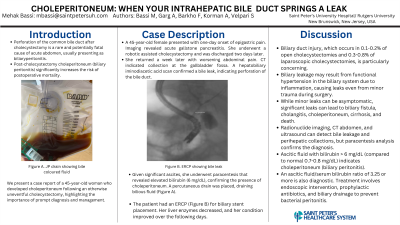
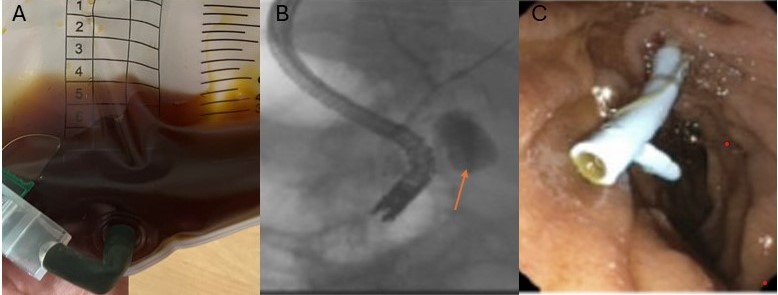
Given significant ascites, she underwent paracentesis that revealed elevated bilirubin (6 mg/dL), confirming the presence of choleperitoneum. A percutaneous drain was placed, draining bilious fluid (Figure A). The patient had an ERCP (Figure B) for biliary stent placement(Figure C). Her liver enzymes decreased, and her condition improved over the following days.
Discussion: Biliary duct injury, which occurs in 0.1-0.2% of open cholecystectomies and 0.3-0.8% of laparoscopic cholecystectomies, is particularly concerning. Biliary leakage may result from functional hypertension in the biliary system due to inflammation, causing leaks even from minor trauma during surgery. While minor leaks can be asymptomatic, significant leaks can lead to biliary fistula, cholangitis, choleperitoneum, cirrhosis, and death. The incidence of choleperitoneum is 0.2% with percutaneous cholecystostomy and 0.3% with open cholecystectomy.
Radionuclide imaging, CT abdomen, and ultrasound can detect bile leakage and perihepatic collections, but paracentesis analysis confirms the diagnosis. Ascitic fluid with bilirubin > 6 mg/dL (compared to normal 0.7-0.8 mg/dL) indicates choleperitoneum (biliary peritonitis). An ascitic fluid/serum bilirubin ratio of 3.25 or more is also diagnostic. Treatment involves endoscopic intervention, prophylactic antibiotics, and biliary drainage to prevent bacterial peritonitis.
Disclosures:
Mehak Bassi, MD1, Archit Garg, MD2, Fadi Barkho, MD2, Sugirdhana Velpari, MD1, Andrew Korman, MD3. P1899 - Choleperitoneum: When Your Intrahepatic Bile Duct Springs a Leak, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ
Introduction: Perforation of the common bile duct after cholecystectomy is a rare and potentially fatal cause of acute abdomen, usually presenting as biliary peritonitis. Post-cholecystectomy choleperitoneum (biliary peritonitis) significantly increases the risk of postoperative mortality. We present a case report of a 45-year-old woman who developed choleperitoneum following an otherwise uneventful cholecystectomy, highlighting the importance of prompt diagnosis and management.
Case Description/Methods: A 45-year-old female presented with one-day onset of epigastric pain, nausea, and vomiting to the emergency. Imaging revealed acute pancreatitis and cholelithiasis. She underwent a robotic-assisted cholecystectomy and was discharged two days later.
She returned a week later with worsening abdominal pain and distension. Imaging indicated severe ascites and post-cholecystectomy changes. CT indicated collection at the gallbladder fossa. A hepatobiliary iminodiacetic acid scan confirmed a bile leak, indicating perforation of the bile duct.
Given significant ascites, she underwent paracentesis that revealed elevated bilirubin (6 mg/dL), confirming the presence of choleperitoneum. A percutaneous drain was placed, draining bilious fluid (Figure A). The patient had an ERCP (Figure B) for biliary stent placement(Figure C). Her liver enzymes decreased, and her condition improved over the following days.
Discussion: Biliary duct injury, which occurs in 0.1-0.2% of open cholecystectomies and 0.3-0.8% of laparoscopic cholecystectomies, is particularly concerning. Biliary leakage may result from functional hypertension in the biliary system due to inflammation, causing leaks even from minor trauma during surgery. While minor leaks can be asymptomatic, significant leaks can lead to biliary fistula, cholangitis, choleperitoneum, cirrhosis, and death. The incidence of choleperitoneum is 0.2% with percutaneous cholecystostomy and 0.3% with open cholecystectomy.
Radionuclide imaging, CT abdomen, and ultrasound can detect bile leakage and perihepatic collections, but paracentesis analysis confirms the diagnosis. Ascitic fluid with bilirubin > 6 mg/dL (compared to normal 0.7-0.8 mg/dL) indicates choleperitoneum (biliary peritonitis). An ascitic fluid/serum bilirubin ratio of 3.25 or more is also diagnostic. Treatment involves endoscopic intervention, prophylactic antibiotics, and biliary drainage to prevent bacterial peritonitis.
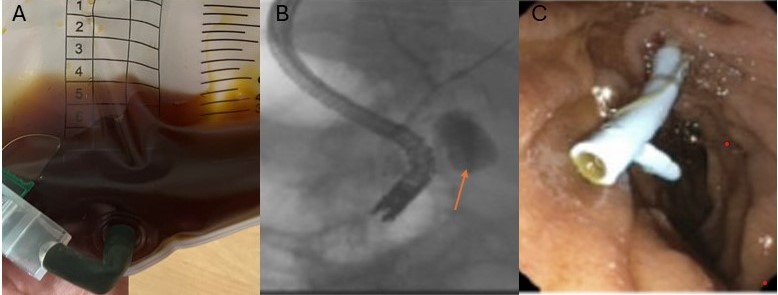
Figure: Figure A: Percutaneous Biliary drain draining bile
Figure B: ERCP image demonstrating bile leak
Figure C: Biliary Stent placement during ERCP
Figure B: ERCP image demonstrating bile leak
Figure C: Biliary Stent placement during ERCP
Disclosures:
Mehak Bassi indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Fadi Barkho indicated no relevant financial relationships.
Sugirdhana Velpari indicated no relevant financial relationships.
Andrew Korman indicated no relevant financial relationships.
Mehak Bassi, MD1, Archit Garg, MD2, Fadi Barkho, MD2, Sugirdhana Velpari, MD1, Andrew Korman, MD3. P1899 - Choleperitoneum: When Your Intrahepatic Bile Duct Springs a Leak, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
