Monday Poster Session
Category: Colon
P1978 - Time Heals All Wounds but Not This One: A Case of an Infiltrating Marjolin Ulcer of the Abdominal Wall Causing Colonic Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CC
Carlo Gabriel Casipit, MD
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Carlo Gabriel Casipit, MD1, Tinsae Anebo, MD1, Hamza Tahir, MBBS, MD2, Phuuwadith Wattanachayakul, MD1, Karecia Byfield, MBBS1, Maxim Barnett, MD1, Jordan Carty, MD1, Mikaela Nikkola Jara-Tantoco, MD1, Elvis Obomanu, MBBS3, Akshay Ratnani, DO1, Anjeli Patel, DO1, Krishna Patel, MD1
1Albert Einstein Medical Center, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Jefferson-Einstein Hospital, Philadelphia, PA
Introduction: Marjolin ulcer is a cutaneous malignancy that occurs because of malignant degeneration of chronic wounds. There is a paucity of reported cases describing Marjolin ulcer as a cause of colonic obstruction.
Case Description/Methods: A 60 year-old male presented to the hospital with a four-week history of intermittent, diffuse, crampy, abdominal pain associated with vomiting, obstipation, and weight loss.
The patient has a history of blunt abdominal trauma from a car accident 20 years ago for which he underwent laparotomy with skin grafting. He was lost to follow-up when he developed a non-healing post-operative abdominal wound with reported fecal drainage. He has no family history of cancer and has not undergone any colonoscopy.
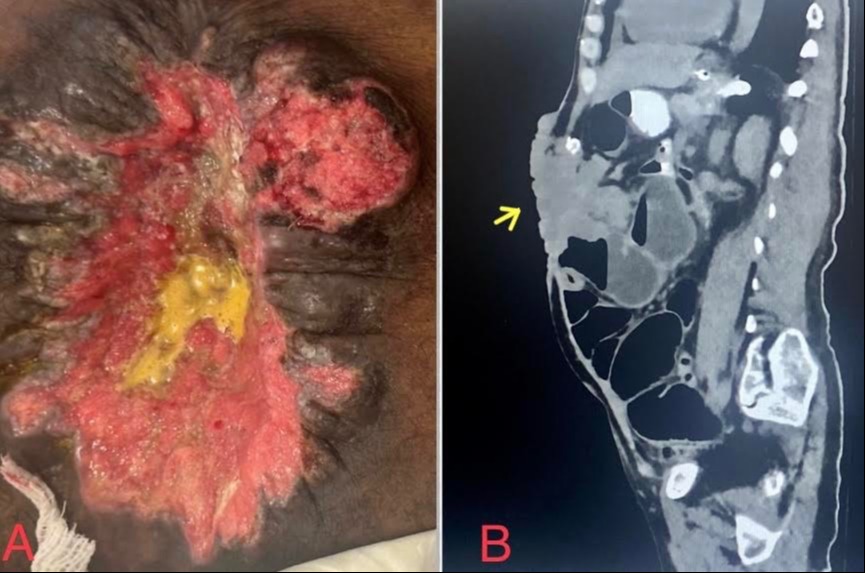
On presentation, he was hemodynamically stable, physical examination showed a chronic, nontender, central wound measuring 16cmx15cmx8cm with an erythematous fibrotic wound bed, papillary borders, and fecal drainage from the wound base. Work-up showed anemia and lactic acidosis. CT of the abdomen with contrast showed enhancing infiltrative heterogeneous mass within the abdominal wall with intraperitoneal extension causing dilation of the proximal colon along with an enterocutaneous fistula.
The patient was placed on NPO, nasogastric tube was inserted, and was given fluids. General Surgery deemed the patient a poor candidate for open abdominal surgery given extensive scarring on his abdominal wall. The gastroenterology team was against endoscopic stenting given the extraluminal nature of the obstruction. Interventional Radiology did a minimally invasive cecostomy to alleviate his symptoms. Biopsy from the abdominal wound showed invasive Squamous Cell Carcinoma. Medical and Radiation Oncology planned chemoradiation. However, before treatment can be initiated, the patient deteriorated rapidly, requiring vasopressors and intubation. Unfortunately, he later succumbed to his illness.
Discussion: Marjolin ulcer reflects malignant degeneration of scar tissue with the time from injury to malignant transformation averaging 20-35 years. The 5-year survival rate is about 30%. High-risk wounds include wounds present for more than three months, increasing size, papillary margins, and chronic discharge. Colonic obstruction in our case was caused by direct intraperitoneal seeding of the abdominal tumor. Treatment goals should focus on early identification of high-risk wounds, prompt biopsy, excision, and strict follow-up with a multidisciplinary approach for the best outcome.
Disclosures:
Carlo Gabriel Casipit, MD1, Tinsae Anebo, MD1, Hamza Tahir, MBBS, MD2, Phuuwadith Wattanachayakul, MD1, Karecia Byfield, MBBS1, Maxim Barnett, MD1, Jordan Carty, MD1, Mikaela Nikkola Jara-Tantoco, MD1, Elvis Obomanu, MBBS3, Akshay Ratnani, DO1, Anjeli Patel, DO1, Krishna Patel, MD1. P1978 - Time Heals All Wounds but Not This One: A Case of an Infiltrating Marjolin Ulcer of the Abdominal Wall Causing Colonic Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Jefferson-Einstein Hospital, Philadelphia, PA
Introduction: Marjolin ulcer is a cutaneous malignancy that occurs because of malignant degeneration of chronic wounds. There is a paucity of reported cases describing Marjolin ulcer as a cause of colonic obstruction.
Case Description/Methods: A 60 year-old male presented to the hospital with a four-week history of intermittent, diffuse, crampy, abdominal pain associated with vomiting, obstipation, and weight loss.
The patient has a history of blunt abdominal trauma from a car accident 20 years ago for which he underwent laparotomy with skin grafting. He was lost to follow-up when he developed a non-healing post-operative abdominal wound with reported fecal drainage. He has no family history of cancer and has not undergone any colonoscopy.
On presentation, he was hemodynamically stable, physical examination showed a chronic, nontender, central wound measuring 16cmx15cmx8cm with an erythematous fibrotic wound bed, papillary borders, and fecal drainage from the wound base. Work-up showed anemia and lactic acidosis. CT of the abdomen with contrast showed enhancing infiltrative heterogeneous mass within the abdominal wall with intraperitoneal extension causing dilation of the proximal colon along with an enterocutaneous fistula.
The patient was placed on NPO, nasogastric tube was inserted, and was given fluids. General Surgery deemed the patient a poor candidate for open abdominal surgery given extensive scarring on his abdominal wall. The gastroenterology team was against endoscopic stenting given the extraluminal nature of the obstruction. Interventional Radiology did a minimally invasive cecostomy to alleviate his symptoms. Biopsy from the abdominal wound showed invasive Squamous Cell Carcinoma. Medical and Radiation Oncology planned chemoradiation. However, before treatment can be initiated, the patient deteriorated rapidly, requiring vasopressors and intubation. Unfortunately, he later succumbed to his illness.
Discussion: Marjolin ulcer reflects malignant degeneration of scar tissue with the time from injury to malignant transformation averaging 20-35 years. The 5-year survival rate is about 30%. High-risk wounds include wounds present for more than three months, increasing size, papillary margins, and chronic discharge. Colonic obstruction in our case was caused by direct intraperitoneal seeding of the abdominal tumor. Treatment goals should focus on early identification of high-risk wounds, prompt biopsy, excision, and strict follow-up with a multidisciplinary approach for the best outcome.
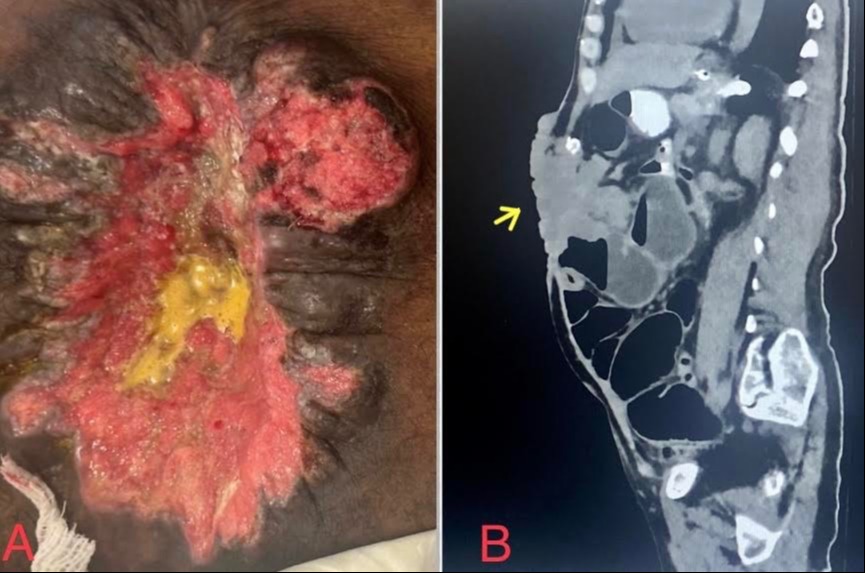
Figure: Image A. Marjolin Ulcer of the abdominal wall characterized by a chronic central wound measuring approximately 16cmx15cmx8cm, with an erythematous fibrotic wound bed, papillary borders, with fecal material oozing out from the base of the wound bed.
Image B. Sagittal view of the CT scan of the Abdomen and Pelvis with contrast showing the abdominal wall tumor (indicated by the yellow arrow) infiltrating intraperitoneally into the bowels causing colonic obstruction.
Image B. Sagittal view of the CT scan of the Abdomen and Pelvis with contrast showing the abdominal wall tumor (indicated by the yellow arrow) infiltrating intraperitoneally into the bowels causing colonic obstruction.
Disclosures:
Carlo Gabriel Casipit indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Hamza Tahir indicated no relevant financial relationships.
Phuuwadith Wattanachayakul indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Maxim Barnett indicated no relevant financial relationships.
Jordan Carty indicated no relevant financial relationships.
Mikaela Nikkola Jara-Tantoco indicated no relevant financial relationships.
Elvis Obomanu indicated no relevant financial relationships.
Akshay Ratnani indicated no relevant financial relationships.
Anjeli Patel indicated no relevant financial relationships.
Krishna Patel indicated no relevant financial relationships.
Carlo Gabriel Casipit, MD1, Tinsae Anebo, MD1, Hamza Tahir, MBBS, MD2, Phuuwadith Wattanachayakul, MD1, Karecia Byfield, MBBS1, Maxim Barnett, MD1, Jordan Carty, MD1, Mikaela Nikkola Jara-Tantoco, MD1, Elvis Obomanu, MBBS3, Akshay Ratnani, DO1, Anjeli Patel, DO1, Krishna Patel, MD1. P1978 - Time Heals All Wounds but Not This One: A Case of an Infiltrating Marjolin Ulcer of the Abdominal Wall Causing Colonic Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
