Monday Poster Session
Category: Colon
P1987 - Dialysis Catheter-Associated Budd Chiari Syndrome Presenting as Ischemic Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sean Dewberry, MD
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Presenting Author(s)
Sean Dewberry, MD, Ali Farhat, MD, Yi-Wei Justin Liu, MD, Andrew Stolz, MD
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Budd Chiari syndrome (BCS) is defined as the occlusion of any of the major hepatic veins or inferior vena cava (IVC). The majority of cases are due to an underlying myeloproliferative disorder causing thrombosis; however, there are case reports describing a malpositioned dialysis catheter as the thrombotic nidus. We now describe a patient with BCS secondary to a thrombosed dialysis catheter presenting with profound hypotension leading to ischemic colitis, a phenomenon not previously reported.
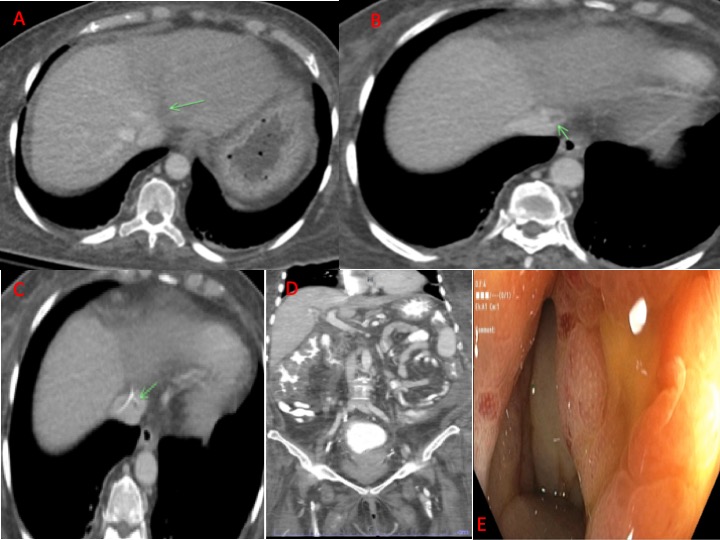
Case Description/Methods: A 63 year old female presented with a three day history of worsening abdominal pain, nonbloody diarrhea, and vomiting. She has end stage renal disease (ESRD) on hemodialysis (HD) through a right internal jugular dialysis catheter, diabetes, and hypertension. She presented with severe hypotension and tachycardia with physical exam revealing abdominal distension, diffuse abdominal pain localizing to the right upper quadrant, and 3+ bilateral pitting leg edema. Labs were notable for a white blood cell count of 6.7k, hemoglobin 11.9, platelets 146k, AP 278, AST 162, ALT 59, INR 1.9, albumin 3, total bilirubin 1.2, direct 0.8 with normal lactate and ammonia. In the ICU, she required three pressors to maintain perfusion. A broad infectious workup was negative. Contrast CT thorax demonstrated a filling defect in the IVC and left hepatic vein near the distal end of the dialysis catheter with decreased attenuation of the left hepatic lobe, concerning for BCS. Contrast CT abdomen/pelvis revealed colonic wall thickening, particularly in watershed segments of the colon, with minimal ascites. She underwent colonoscopy that demonstrated diffuse areas of submucosal hemorrhage and friability, consistent with ischemia. Of note, the patient similarly presented four months prior and a colonoscopy demonstrated normal mucosa without BCS being identified. The patient was started on anticoagulation with improvement in her symptoms and labs. Her catheter was replaced several days later and she was discharged in stable condition.
Discussion: Dialysis catheter-associated BCS has rarely been reported in the literature and clinical manifestations are typically related to liver-related complications. Over 70% of patients with ESRD initiate HD through a central catheter, highlighting the potential incidence of this phenomenon. In those patients presenting with shock and ischemic colitis with a dialysis catheter, catheter associated thrombosis must be considered in the differential diagnosis.
Disclosures:
Sean Dewberry, MD, Ali Farhat, MD, Yi-Wei Justin Liu, MD, Andrew Stolz, MD. P1987 - Dialysis Catheter-Associated Budd Chiari Syndrome Presenting as Ischemic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Budd Chiari syndrome (BCS) is defined as the occlusion of any of the major hepatic veins or inferior vena cava (IVC). The majority of cases are due to an underlying myeloproliferative disorder causing thrombosis; however, there are case reports describing a malpositioned dialysis catheter as the thrombotic nidus. We now describe a patient with BCS secondary to a thrombosed dialysis catheter presenting with profound hypotension leading to ischemic colitis, a phenomenon not previously reported.
Case Description/Methods: A 63 year old female presented with a three day history of worsening abdominal pain, nonbloody diarrhea, and vomiting. She has end stage renal disease (ESRD) on hemodialysis (HD) through a right internal jugular dialysis catheter, diabetes, and hypertension. She presented with severe hypotension and tachycardia with physical exam revealing abdominal distension, diffuse abdominal pain localizing to the right upper quadrant, and 3+ bilateral pitting leg edema. Labs were notable for a white blood cell count of 6.7k, hemoglobin 11.9, platelets 146k, AP 278, AST 162, ALT 59, INR 1.9, albumin 3, total bilirubin 1.2, direct 0.8 with normal lactate and ammonia. In the ICU, she required three pressors to maintain perfusion. A broad infectious workup was negative. Contrast CT thorax demonstrated a filling defect in the IVC and left hepatic vein near the distal end of the dialysis catheter with decreased attenuation of the left hepatic lobe, concerning for BCS. Contrast CT abdomen/pelvis revealed colonic wall thickening, particularly in watershed segments of the colon, with minimal ascites. She underwent colonoscopy that demonstrated diffuse areas of submucosal hemorrhage and friability, consistent with ischemia. Of note, the patient similarly presented four months prior and a colonoscopy demonstrated normal mucosa without BCS being identified. The patient was started on anticoagulation with improvement in her symptoms and labs. Her catheter was replaced several days later and she was discharged in stable condition.
Discussion: Dialysis catheter-associated BCS has rarely been reported in the literature and clinical manifestations are typically related to liver-related complications. Over 70% of patients with ESRD initiate HD through a central catheter, highlighting the potential incidence of this phenomenon. In those patients presenting with shock and ischemic colitis with a dialysis catheter, catheter associated thrombosis must be considered in the differential diagnosis.
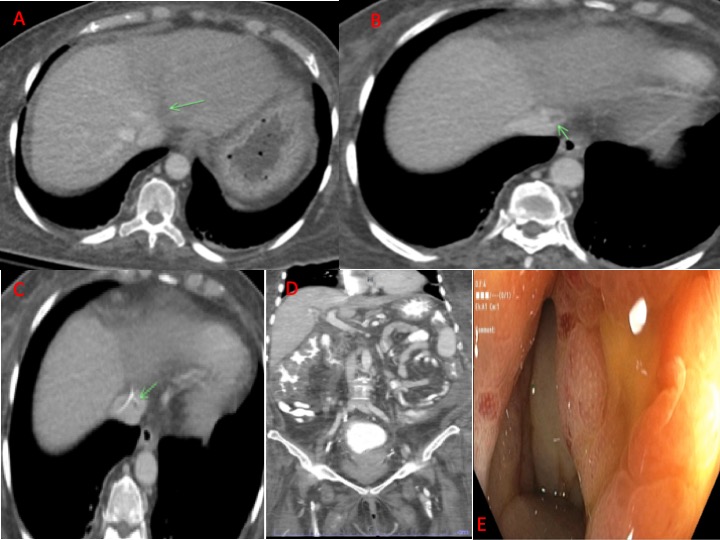
Figure: A: Contrast-enhanced abdominal CT axial view; Non-opacification of the left hepatic vein (green arrow) relative to the middle and right hepatic vein compatible with occlusive thrombus. There is associated hypoattenuation of the left hepatic lobe with respect to the right. B/C: Contrast-enhanced abdominal CT axial views; Partially occlusive filling defect in the inferior vena cava (green arrow, B) which was noted to abut the distal tip of a right internal jugular dialysis catheter (green arrow, C). D: Abdominal CT with oral and IV contrast coronal view; Diffuse colonic wall thickening compatible with colitis. E: Colonoscopy with example of scattered colonic ulcerations in the ascending colon surrounded by erythematous, edematous colonic mucosa.
Disclosures:
Sean Dewberry indicated no relevant financial relationships.
Ali Farhat indicated no relevant financial relationships.
Yi-Wei Justin Liu indicated no relevant financial relationships.
Andrew Stolz indicated no relevant financial relationships.
Sean Dewberry, MD, Ali Farhat, MD, Yi-Wei Justin Liu, MD, Andrew Stolz, MD. P1987 - Dialysis Catheter-Associated Budd Chiari Syndrome Presenting as Ischemic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
