Monday Poster Session
Category: Colon
P2048 - A Case of Severe Campylobacter Colitis in an Immunosuppressed Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Patrick J. Graf, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Patrick J. Graf, MD, Dana M. Blyth, MD, Chelsea M. Forbes, MD, Jared Magee, DO, MPH, John M. Curtin, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Campylobacter infection, most commonly C. jejuni, is a leading cause of acute bacterial diarrhea. It is usually acquired via contaminated food products such as undercooked poultry and typically results in a self-limited enteritis. Uncommonly, severe disease including colitis, pseudoappendicitis, bacteremia (< 1% of cases), and even death may be seen, especially among immunosuppressed patients. We present a case of C. jejuni infection presenting as severe colitis and bacteremia in an immunosuppressed host.
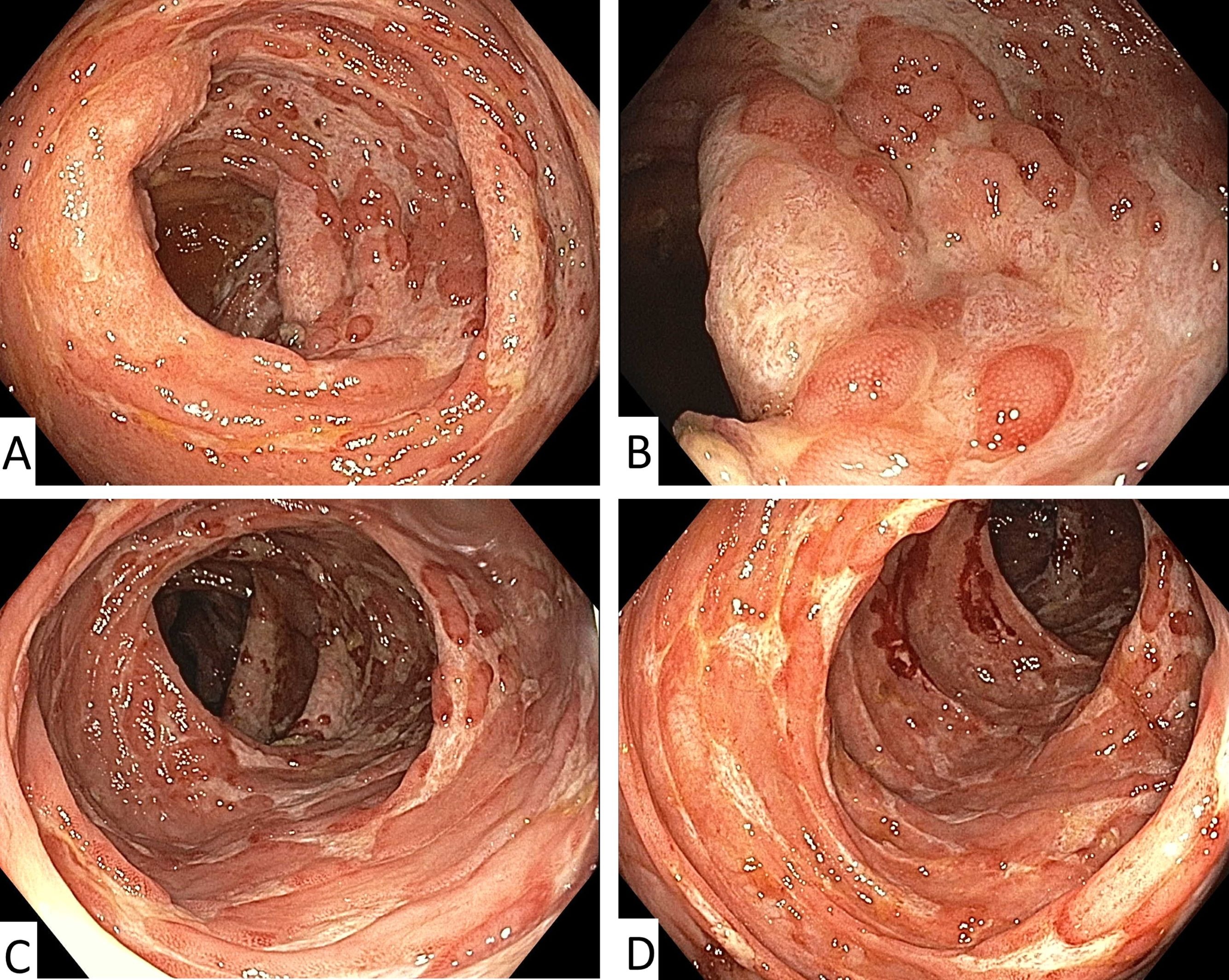
Case Description/Methods: A 74-year-old man with CLL on ibrutinib presented with fever, hypotension, and 4 days of non-bloody diarrhea after eating undercooked chicken. C. jejuni grew on initial blood cultures. Stool polymerase chain reaction (PCR) testing was positive for Campylobacter, toxin and PCR testing for C. difficile was negative. Azithromycin therapy resulted in initial improvements in blood pressure, diarrhea, and blood culture clearance. However, on day 8 he developed a rising leukocytosis, new bloody diarrhea and his hemoglobin fell from 10.0 to 5.8 g/dL over 4 days despite blood transfusions, ultimately requiring 10 units. Colonoscopy demonstrated erythema, friability, shallow ulcers, and exudate throughout the ascending colon. Biopsy showed non-specific inflammation with ulceration but no evidence of cytomegalovirus infection or inflammatory bowel disease. He was switched to meropenem and subsequently had gradual improvement. Testing of the C. jejuni blood isolate ultimately confirmed susceptibility to azithromycin and meropenem. In total, he completed 10 days of azithromycin and 7 days of meropenem with complete resolution of symptoms.
Discussion: This report highlights an unusual case of severe Campylobacter infection presenting as colitis and bacteremia in an immunosuppressed patient. Typically, C. jejuni manifests as an acute, self-limited diarrheal illness affecting the small intestine. This scenario presented unique challenges to clinical management, as the degree of blood loss and relapsed symptoms raised concerns for potential resistance and infection progression in the setting of immunocompromise. Antibiotic resistance remains common, with fluoroquinolone resistance rates exceeding 20% and 80% in the U.S. and Southeast Asia, respectively. Fortunately, less than 5% of U.S. isolates are azithromycin resistant. Carbapenems remain almost universally effective, making them a good empiric option in patients with severe disease not responding to macrolide therapy.
Disclosures:
Patrick J. Graf, MD, Dana M. Blyth, MD, Chelsea M. Forbes, MD, Jared Magee, DO, MPH, John M. Curtin, MD. P2048 - A Case of Severe <i>Campylobacter</i> Colitis in an Immunosuppressed Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Campylobacter infection, most commonly C. jejuni, is a leading cause of acute bacterial diarrhea. It is usually acquired via contaminated food products such as undercooked poultry and typically results in a self-limited enteritis. Uncommonly, severe disease including colitis, pseudoappendicitis, bacteremia (< 1% of cases), and even death may be seen, especially among immunosuppressed patients. We present a case of C. jejuni infection presenting as severe colitis and bacteremia in an immunosuppressed host.
Case Description/Methods: A 74-year-old man with CLL on ibrutinib presented with fever, hypotension, and 4 days of non-bloody diarrhea after eating undercooked chicken. C. jejuni grew on initial blood cultures. Stool polymerase chain reaction (PCR) testing was positive for Campylobacter, toxin and PCR testing for C. difficile was negative. Azithromycin therapy resulted in initial improvements in blood pressure, diarrhea, and blood culture clearance. However, on day 8 he developed a rising leukocytosis, new bloody diarrhea and his hemoglobin fell from 10.0 to 5.8 g/dL over 4 days despite blood transfusions, ultimately requiring 10 units. Colonoscopy demonstrated erythema, friability, shallow ulcers, and exudate throughout the ascending colon. Biopsy showed non-specific inflammation with ulceration but no evidence of cytomegalovirus infection or inflammatory bowel disease. He was switched to meropenem and subsequently had gradual improvement. Testing of the C. jejuni blood isolate ultimately confirmed susceptibility to azithromycin and meropenem. In total, he completed 10 days of azithromycin and 7 days of meropenem with complete resolution of symptoms.
Discussion: This report highlights an unusual case of severe Campylobacter infection presenting as colitis and bacteremia in an immunosuppressed patient. Typically, C. jejuni manifests as an acute, self-limited diarrheal illness affecting the small intestine. This scenario presented unique challenges to clinical management, as the degree of blood loss and relapsed symptoms raised concerns for potential resistance and infection progression in the setting of immunocompromise. Antibiotic resistance remains common, with fluoroquinolone resistance rates exceeding 20% and 80% in the U.S. and Southeast Asia, respectively. Fortunately, less than 5% of U.S. isolates are azithromycin resistant. Carbapenems remain almost universally effective, making them a good empiric option in patients with severe disease not responding to macrolide therapy.
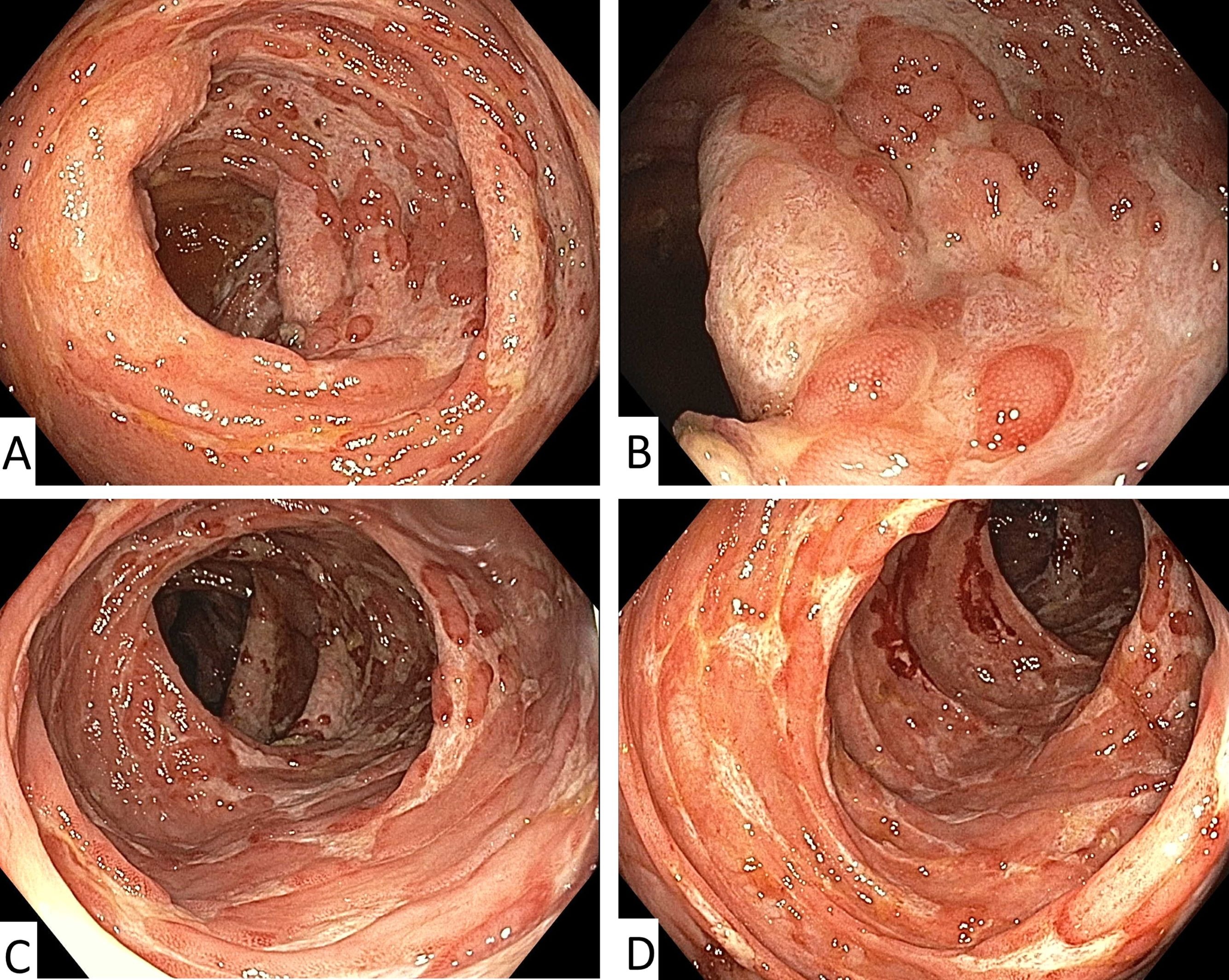
Figure: Figures A – D: Colonoscopy images demonstrating erythema, friability, mucous exudate, and shallow ulceration throughout the cecum and ascending colon extending to the hepatic flexure (A-D)
Disclosures:
Patrick Graf indicated no relevant financial relationships.
Dana Blyth indicated no relevant financial relationships.
Chelsea Forbes indicated no relevant financial relationships.
Jared Magee indicated no relevant financial relationships.
John Curtin indicated no relevant financial relationships.
Patrick J. Graf, MD, Dana M. Blyth, MD, Chelsea M. Forbes, MD, Jared Magee, DO, MPH, John M. Curtin, MD. P2048 - A Case of Severe <i>Campylobacter</i> Colitis in an Immunosuppressed Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
