Monday Poster Session
Category: Colon
P2058 - A Case of Severe ICI-Colitis With Suprainfection
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sebastian S. Dobrow, MD, MPH
University of Chicago Medicine
Chicago, IL
Presenting Author(s)
Sebastian S. Dobrow, MD, MPH1, Grace E. Kim, MD2, Bradford Chong, MD3
1University of Chicago Medicine, Chicago, IL; 2Center for Endoscopic Research and Therapeutics (CERT), University of Chicago, Chicago, IL; 3University of Chicago Medical Center, Chicago, IL
Introduction: Immune checkpoint inhibitors (ICIs) are becoming widely used cancer therapies, but alongside them a spectrum of immune-related adverse events (irAEs) have emerged. IrAEs can affect nearly every organ system, with up to 50% having GI involvement. We present a complex case of a severe ICI colitis that initially improved with prompt management but ultimately led to death.
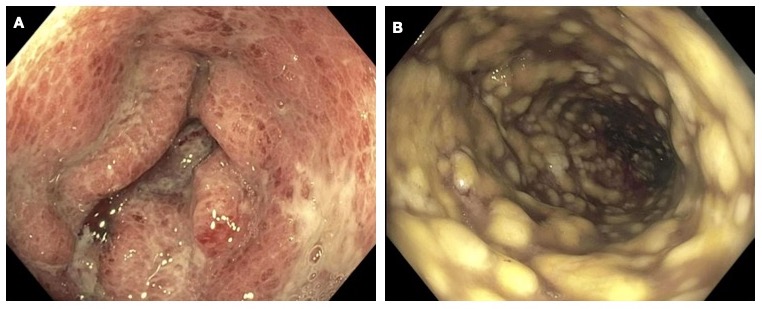
Case Description/Methods: An 81-year-old male with metastatic melanoma on nivolumab and relatlimab with biopsy-proven ICI colitis (Figure 1A) on prednisone initially presented to the hospital with diarrhea. He was positive for Clostridium difficile (C. diff) and was treated with a full course of antibiotics. He presented again a few days later with hematochezia and shock requiring pressors. GI pathogen panel was negative on two separate samples, and he underwent a flexible sigmoidoscopy with biopsies that confirmed ICI colitis as well as CMV colitis. He was then started on infliximab and ganciclovir with initial symptom improvement. Several days after the second infliximab dose, however, the patient developed hematochezia again prompting a repeat colonoscopy. This showed severe diffuse pseudomembranous colitis in the entire colon concerning for C. diff infection (Figure 1B). GI pathogen panel confirmed C. diff infection, and the patient was started on fidaxomicin. Unfortunately, due to multiorgan failure and severe deconditioning, the patient transitioned to comfort care and passed away.
Discussion: ICI colitis is graded based on severity, with grade 2 and above requiring endoscopic evaluation. Severe colitis (i.e., grade 3 or 4) may require steroid therapy in addition to infliximab or vedolizumab, usually dosed at 0, 2, and 6 weeks, and patients typically respond within a week. Nonresponse to therapy necessitates a prompt workup of other causes for continued diarrhea, especially infectious etiologies, as these patients are heavily immunosuppressed and are prone to severe sequelae of infection. This case highlights the importance of avoiding anchoring bias and having a low threshold for an endoscopic evaluation when a patient’s clinical course does not make sense, especially in immunocompromised patients.
Disclosures:
Sebastian S. Dobrow, MD, MPH1, Grace E. Kim, MD2, Bradford Chong, MD3. P2058 - A Case of Severe ICI-Colitis With Suprainfection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Chicago Medicine, Chicago, IL; 2Center for Endoscopic Research and Therapeutics (CERT), University of Chicago, Chicago, IL; 3University of Chicago Medical Center, Chicago, IL
Introduction: Immune checkpoint inhibitors (ICIs) are becoming widely used cancer therapies, but alongside them a spectrum of immune-related adverse events (irAEs) have emerged. IrAEs can affect nearly every organ system, with up to 50% having GI involvement. We present a complex case of a severe ICI colitis that initially improved with prompt management but ultimately led to death.
Case Description/Methods: An 81-year-old male with metastatic melanoma on nivolumab and relatlimab with biopsy-proven ICI colitis (Figure 1A) on prednisone initially presented to the hospital with diarrhea. He was positive for Clostridium difficile (C. diff) and was treated with a full course of antibiotics. He presented again a few days later with hematochezia and shock requiring pressors. GI pathogen panel was negative on two separate samples, and he underwent a flexible sigmoidoscopy with biopsies that confirmed ICI colitis as well as CMV colitis. He was then started on infliximab and ganciclovir with initial symptom improvement. Several days after the second infliximab dose, however, the patient developed hematochezia again prompting a repeat colonoscopy. This showed severe diffuse pseudomembranous colitis in the entire colon concerning for C. diff infection (Figure 1B). GI pathogen panel confirmed C. diff infection, and the patient was started on fidaxomicin. Unfortunately, due to multiorgan failure and severe deconditioning, the patient transitioned to comfort care and passed away.
Discussion: ICI colitis is graded based on severity, with grade 2 and above requiring endoscopic evaluation. Severe colitis (i.e., grade 3 or 4) may require steroid therapy in addition to infliximab or vedolizumab, usually dosed at 0, 2, and 6 weeks, and patients typically respond within a week. Nonresponse to therapy necessitates a prompt workup of other causes for continued diarrhea, especially infectious etiologies, as these patients are heavily immunosuppressed and are prone to severe sequelae of infection. This case highlights the importance of avoiding anchoring bias and having a low threshold for an endoscopic evaluation when a patient’s clinical course does not make sense, especially in immunocompromised patients.
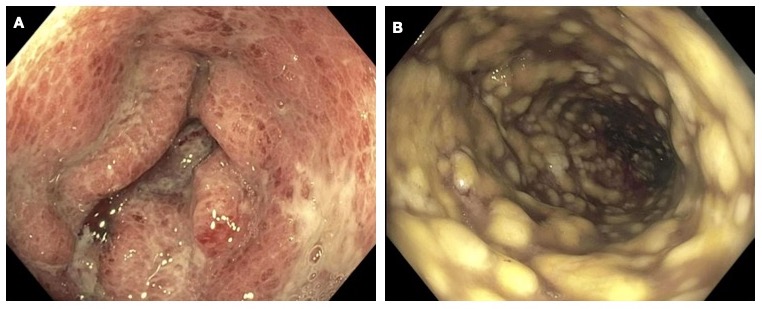
Figure: Figure 1. (A) Colonic mucosal inflammation and ulceration in immune checkpoint inhibitor-colitis. (B) Severe diffuse pseudomembranous colitis in setting of Clostridium difficile infection.
Disclosures:
Sebastian Dobrow indicated no relevant financial relationships.
Grace Kim indicated no relevant financial relationships.
Bradford Chong indicated no relevant financial relationships.
Sebastian S. Dobrow, MD, MPH1, Grace E. Kim, MD2, Bradford Chong, MD3. P2058 - A Case of Severe ICI-Colitis With Suprainfection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
