Monday Poster Session
Category: Colon
P2095 - A Case for Gastrointestinal Specific Polyps in Neurofibromatosis-1
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Jonathan Rozenberg, DO, MPH
Carilion Clinic
Roanoke, VA
Presenting Author(s)
Jonathan Rozenberg, DO, MPH1, Adil Mir, MD1, Klaus Monkemuller, MD, PhD2, Bara El Kurdi, MD2, Douglas Grider, MD2
1Carilion Clinic, Roanoke, VA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Gastrointestinal (GI) tract associations of Neurofibromatosis-1 (NF-1) are well documented in the literature and vary from common benign lesions to rare malignancies. GI stromal tumors (GIST) and peripheral nerve sheath tumors are described as the most common forms of GI tract involvement by NF-1, respectively. Other types of lesions, such as juvenile-like (inflammatory/hyperplastic) mucosal polyps (JLIHMP) and/or inflammatory fibroid mucosal polyps (IFMP) are rarely reported within the current body of literature. We present a rare case of both JLIHMP and IFMP found on colonoscopy in an asymptomatic NF-1 patient.
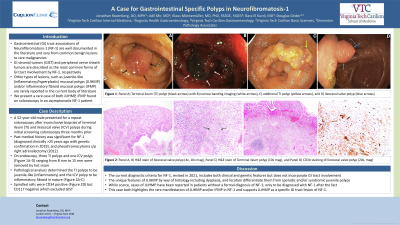
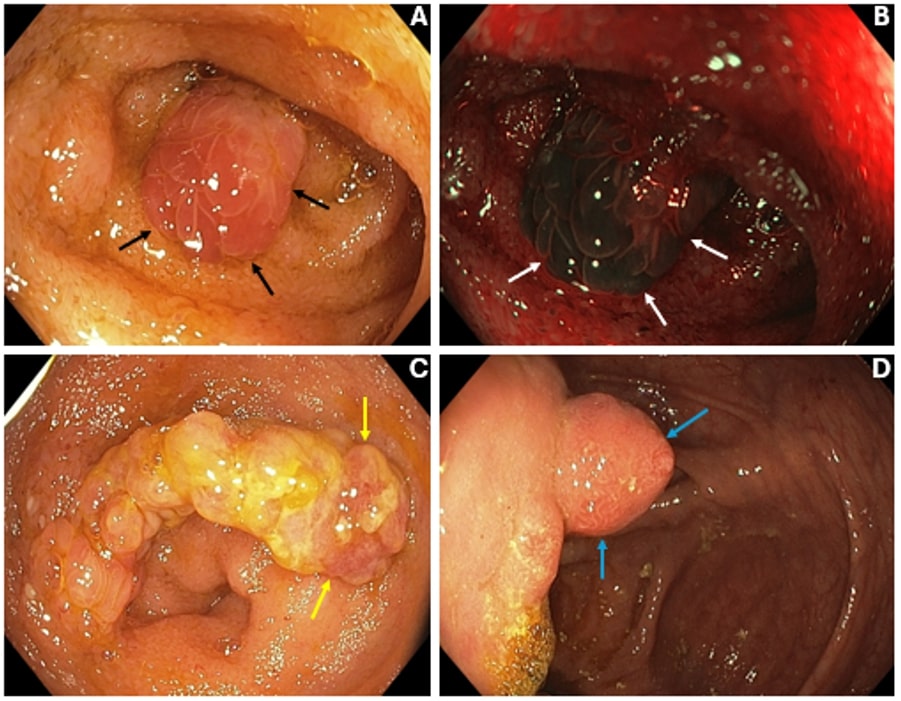
Case Description/Methods: A 52-year-old male presented for a repeat colonoscopy after inconclusive biopsies of terminal ileum (TI) and ileocecal valve (ICV) polyps during initial screening colonoscopy three months prior. Past medical history was significant for NF-1 (diagnosed clinically more than 25 years ago with genetic confirmation in 2019), and pheochromocytoma status post right adrenalectomy (2012). On endoscopy, three TI polyps and one ICV polyp (Figure 1) ranging from 8 mm to 15 mm were removed by hot snare. Pathological analysis determined the TI polyps to be juvenile-like (inflammatory) and the ICV polyp to be inflammatory fibroid in nature. Spindled cells were CD34 positive but CD117 negative which excluded GIST.
Discussion: The current diagnostic criteria for NF-1, revised in 2021, includes both clinical and genetic features but does not incorporate GI tract involvement. The unique features of JLIHMP by way of histology (e.g., variation of appearance and/or greater predominance of inflammatory stroma) including dysplasia (e.g., frequently without any dysplastic characteristics), and location (e.g., small bowel, proximal colon) differentiate them from sporadic and/or syndromic juvenile polyps which points towards a disease specific process. Of note, while scarce, cases of JLIHMP have been reported in patients without a formal diagnosis of NF-1; only to be diagnosed with NF-1 after the fact. Along the same breadth, IFMP in NF-1 have only been seen in only a handful of cases. This case both highlights the rare manifestation of JLIHMP and/or IFMP in NF-1 and contributes to the body of literature aiming to designate JLIHMP as a specific GI tract lesion of NF-1.
Disclosures:
Jonathan Rozenberg, DO, MPH1, Adil Mir, MD1, Klaus Monkemuller, MD, PhD2, Bara El Kurdi, MD2, Douglas Grider, MD2. P2095 - A Case for Gastrointestinal Specific Polyps in Neurofibromatosis-1, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Carilion Clinic, Roanoke, VA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Gastrointestinal (GI) tract associations of Neurofibromatosis-1 (NF-1) are well documented in the literature and vary from common benign lesions to rare malignancies. GI stromal tumors (GIST) and peripheral nerve sheath tumors are described as the most common forms of GI tract involvement by NF-1, respectively. Other types of lesions, such as juvenile-like (inflammatory/hyperplastic) mucosal polyps (JLIHMP) and/or inflammatory fibroid mucosal polyps (IFMP) are rarely reported within the current body of literature. We present a rare case of both JLIHMP and IFMP found on colonoscopy in an asymptomatic NF-1 patient.
Case Description/Methods: A 52-year-old male presented for a repeat colonoscopy after inconclusive biopsies of terminal ileum (TI) and ileocecal valve (ICV) polyps during initial screening colonoscopy three months prior. Past medical history was significant for NF-1 (diagnosed clinically more than 25 years ago with genetic confirmation in 2019), and pheochromocytoma status post right adrenalectomy (2012). On endoscopy, three TI polyps and one ICV polyp (Figure 1) ranging from 8 mm to 15 mm were removed by hot snare. Pathological analysis determined the TI polyps to be juvenile-like (inflammatory) and the ICV polyp to be inflammatory fibroid in nature. Spindled cells were CD34 positive but CD117 negative which excluded GIST.
Discussion: The current diagnostic criteria for NF-1, revised in 2021, includes both clinical and genetic features but does not incorporate GI tract involvement. The unique features of JLIHMP by way of histology (e.g., variation of appearance and/or greater predominance of inflammatory stroma) including dysplasia (e.g., frequently without any dysplastic characteristics), and location (e.g., small bowel, proximal colon) differentiate them from sporadic and/or syndromic juvenile polyps which points towards a disease specific process. Of note, while scarce, cases of JLIHMP have been reported in patients without a formal diagnosis of NF-1; only to be diagnosed with NF-1 after the fact. Along the same breadth, IFMP in NF-1 have only been seen in only a handful of cases. This case both highlights the rare manifestation of JLIHMP and/or IFMP in NF-1 and contributes to the body of literature aiming to designate JLIHMP as a specific GI tract lesion of NF-1.
Figure: Figure 1: Panel A) Terminal ileum (TI) polyp (black arrows) with B) narrow banding imaging (white arrows), C) additional TI polyp (yellow arrows), and D) Ileocecal valve polyp (blue arrows)
Disclosures:
Jonathan Rozenberg indicated no relevant financial relationships.
Adil Mir indicated no relevant financial relationships.
Klaus Monkemuller indicated no relevant financial relationships.
Bara El Kurdi indicated no relevant financial relationships.
Douglas Grider indicated no relevant financial relationships.
Jonathan Rozenberg, DO, MPH1, Adil Mir, MD1, Klaus Monkemuller, MD, PhD2, Bara El Kurdi, MD2, Douglas Grider, MD2. P2095 - A Case for Gastrointestinal Specific Polyps in Neurofibromatosis-1, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
