Monday Poster Session
Category: Colorectal Cancer Prevention
P2107 - Uncovering Hidden Risks: Exploring Adenoma Detection Rates in Adult Colonoscopy Patients Within a Large Community Setting
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lawrence Zhou, MD
The University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Lawrence Zhou, MD1, Aastha V. Bharwad, MD2, John Thesing, DO2, Joseph Odeyemi, MD2, Noufil Adnan, MD2, Hayrettin Okut, PhD2, Nathan Tofteland, MD2
1The University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS
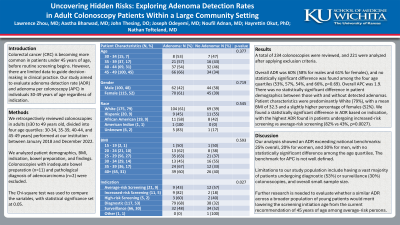
Introduction: Colorectal cancer (CRC) is becoming more common in patients under 45 years of age, before routine screening begins. However, there are limited data to guide decision-making in clinical practice. Our study aims to evaluate adenoma detection rate (ADR) and adenoma per colonoscopy (APC) in individuals 30-49 years of age regardless of indication.
Methods: We retrospectively reviewed colonoscopies in adults (≥30 to 49 years old, divided into four age quartiles: 30-34, 35-39, 40-44, and 45-49 years) performed at our institution between January 2018 and December 2022. We analyzed patient demographics, BMI, indication, bowel preparation, and findings. Colonoscopies with inadequate bowel preparation (n=11) and pathological diagnosis of adenocarcinoma (n=2) were excluded. The Chi-square test was used to compare the variables, with statistical significance set at 0.05.
Results: A total of 234 colonoscopies were reviewed, and 221 were analyzed after applying exclusion criteria. Overall ADR was 60% (58% for males and 61% for females), and no statistically significant difference was found among the four age quartiles (53%, 57%, 54%, and 66%, p=0.69). Overall APC was 1.9. There was no statistically significant difference in patient demographics between those with and without detected adenomas (Table). Patient characteristics were predominantly White (79%), with a mean BMI of 32.3 and a slightly higher percentage of females (52%). We found a statistically significant difference in ADR based on indication, with the highest ADR found in patients undergoing increased-risk screening compared to average-risk screening (82% vs 43%, p=0.0027).
Discussion: Our analysis of younger individuals undergoing colonoscopy showed ADR exceeding national benchmarks: 25% overall, 20% for women, and 30% for men, with no statistically significant difference among the age quartiles. The benchmark for APC is not well defined. Limitations to our study population include having a vast majority of patients undergoing diagnostic (53%) or surveillance (30%) colonoscopies, and overall having a small sample size. Further research is needed to evaluate whether a similar ADR across a broader population of young patients would merit lowering the screening initiation age from the current recommendation of 45 years of age among average-risk persons.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lawrence Zhou, MD1, Aastha V. Bharwad, MD2, John Thesing, DO2, Joseph Odeyemi, MD2, Noufil Adnan, MD2, Hayrettin Okut, PhD2, Nathan Tofteland, MD2. P2107 - Uncovering Hidden Risks: Exploring Adenoma Detection Rates in Adult Colonoscopy Patients Within a Large Community Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS
Introduction: Colorectal cancer (CRC) is becoming more common in patients under 45 years of age, before routine screening begins. However, there are limited data to guide decision-making in clinical practice. Our study aims to evaluate adenoma detection rate (ADR) and adenoma per colonoscopy (APC) in individuals 30-49 years of age regardless of indication.
Methods: We retrospectively reviewed colonoscopies in adults (≥30 to 49 years old, divided into four age quartiles: 30-34, 35-39, 40-44, and 45-49 years) performed at our institution between January 2018 and December 2022. We analyzed patient demographics, BMI, indication, bowel preparation, and findings. Colonoscopies with inadequate bowel preparation (n=11) and pathological diagnosis of adenocarcinoma (n=2) were excluded. The Chi-square test was used to compare the variables, with statistical significance set at 0.05.
Results: A total of 234 colonoscopies were reviewed, and 221 were analyzed after applying exclusion criteria. Overall ADR was 60% (58% for males and 61% for females), and no statistically significant difference was found among the four age quartiles (53%, 57%, 54%, and 66%, p=0.69). Overall APC was 1.9. There was no statistically significant difference in patient demographics between those with and without detected adenomas (Table). Patient characteristics were predominantly White (79%), with a mean BMI of 32.3 and a slightly higher percentage of females (52%). We found a statistically significant difference in ADR based on indication, with the highest ADR found in patients undergoing increased-risk screening compared to average-risk screening (82% vs 43%, p=0.0027).
Discussion: Our analysis of younger individuals undergoing colonoscopy showed ADR exceeding national benchmarks: 25% overall, 20% for women, and 30% for men, with no statistically significant difference among the age quartiles. The benchmark for APC is not well defined. Limitations to our study population include having a vast majority of patients undergoing diagnostic (53%) or surveillance (30%) colonoscopies, and overall having a small sample size. Further research is needed to evaluate whether a similar ADR across a broader population of young patients would merit lowering the screening initiation age from the current recommendation of 45 years of age among average-risk persons.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lawrence Zhou indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
Joseph Odeyemi indicated no relevant financial relationships.
Noufil Adnan indicated no relevant financial relationships.
Hayrettin Okut indicated no relevant financial relationships.
Nathan Tofteland indicated no relevant financial relationships.
Lawrence Zhou, MD1, Aastha V. Bharwad, MD2, John Thesing, DO2, Joseph Odeyemi, MD2, Noufil Adnan, MD2, Hayrettin Okut, PhD2, Nathan Tofteland, MD2. P2107 - Uncovering Hidden Risks: Exploring Adenoma Detection Rates in Adult Colonoscopy Patients Within a Large Community Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
