Monday Poster Session
Category: Colorectal Cancer Prevention
P2135 - Measuring Mucosal Inspection Time to Determine Optimal Withdrawal Time in Diagnostic and Screening Colonoscopy: A Mixed Methods Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Samuel H. Cheong, DO
Banner - University of Arizona
Tucson, AZ
Presenting Author(s)
Samuel H. Cheong, DO1, Amar Vedamurthy, MD, MSCI, MRCP (UK)2, Elise Le Cam, MD1, Akira Folk, DO1, Brendan Andres, MD3, Malini Chauhan, MD4, Shivanand Bomman, MD4, Mahak Chauhan, MD1, Avin Aggarwal, MD5, Joshua Melson, MD4
1Banner - University of Arizona, Tucson, AZ; 2Virginia Mason Franciscan Health, Tucson, AZ; 3University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 4University of Arizona College of Medicine, Tucson, AZ; 5University of Arizona, Tucson, AZ
Introduction: Withdrawal time (WT) and adenoma detection rate (ADR) are quality indicators for colonoscopy. However, most studies on WT do not account for the time spent removing polyps, leading to incomplete assessments of inspection times. Thus, there is a need for an objective tool to measure mucosal inspection time (MIT) during withdrawal to reflect the effective examination time accurately. Our novel quality indicator was evaluated based on real-time measurement of polypectomy time (PT) and assessed the impact of adjusted WT on ADR.
Methods: This mixed methods study was conducted at two academic hospitals. The prospective study included asymptomatic patients who had colonoscopy with polypectomy to quantify PT (measured with a stopwatch). MIT was calculated as: [WT – (Median PT x number of adenomas per colonoscopy)]. ADR and adenomas per colonoscopy (APC) were calculated at two intervals of WT and MIT. Multilevel regression was used to analyze longitudinal data. The retrospective cohort included patients who underwent upfront screening colonoscopy or colonoscopy after a positive stool mt-sDNA test. Patient and polyp characteristics affecting WT were recorded.
Results: The prospective cohort included 201 patients with 494 polyps removed. PT was similar for males and females. The polypectomy via hot snare had a longer PT than cold snare and cold forceps. Right and left colon polyps had similar PT. Polyps < 10 mm had shorter PT than polyps ≥ 10 mm. There was no significant variability among five endoscopists; the PT of fellows was 0.3 minutes longer than attendings. The retrospective cohort included 1204 patients; 306 underwent colonoscopy after a positive mt-sDNA test and 898 underwent upfront colonoscopy. MIT was calculated using a median PT of 0.6 minutes. In the mt-sDNA group, the ADR for WT intervals of 6-9 minutes was 38% and 50% for 9-12 minutes. Using MIT, the ADR was better for interval 9-12 (61%). In the upfront colonoscopy cohort, MIT improved ADR compared to WT in both 6-9 (20% vs 23%) and 9-12 (42% vs 47%). Extending MIT to > 9 minutes resulted in a 73% (95% CI 1.29-2.32) greater likelihood to identify adenomas in the upfront cohort and a 37% improvement in ADR in the mt-sDNA cohort compared to 6-9 minutes.
Discussion: MIT as a quality indicator for colonoscopy provides a more accurate assessment of withdrawal time’s impact on ADR. Extending MIT beyond 9 minutes significantly enhances adenoma detection in upfront screening and diagnostic cohorts.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Samuel H. Cheong, DO1, Amar Vedamurthy, MD, MSCI, MRCP (UK)2, Elise Le Cam, MD1, Akira Folk, DO1, Brendan Andres, MD3, Malini Chauhan, MD4, Shivanand Bomman, MD4, Mahak Chauhan, MD1, Avin Aggarwal, MD5, Joshua Melson, MD4. P2135 - Measuring Mucosal Inspection Time to Determine Optimal Withdrawal Time in Diagnostic and Screening Colonoscopy: A Mixed Methods Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Banner - University of Arizona, Tucson, AZ; 2Virginia Mason Franciscan Health, Tucson, AZ; 3University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 4University of Arizona College of Medicine, Tucson, AZ; 5University of Arizona, Tucson, AZ
Introduction: Withdrawal time (WT) and adenoma detection rate (ADR) are quality indicators for colonoscopy. However, most studies on WT do not account for the time spent removing polyps, leading to incomplete assessments of inspection times. Thus, there is a need for an objective tool to measure mucosal inspection time (MIT) during withdrawal to reflect the effective examination time accurately. Our novel quality indicator was evaluated based on real-time measurement of polypectomy time (PT) and assessed the impact of adjusted WT on ADR.
Methods: This mixed methods study was conducted at two academic hospitals. The prospective study included asymptomatic patients who had colonoscopy with polypectomy to quantify PT (measured with a stopwatch). MIT was calculated as: [WT – (Median PT x number of adenomas per colonoscopy)]. ADR and adenomas per colonoscopy (APC) were calculated at two intervals of WT and MIT. Multilevel regression was used to analyze longitudinal data. The retrospective cohort included patients who underwent upfront screening colonoscopy or colonoscopy after a positive stool mt-sDNA test. Patient and polyp characteristics affecting WT were recorded.
Results: The prospective cohort included 201 patients with 494 polyps removed. PT was similar for males and females. The polypectomy via hot snare had a longer PT than cold snare and cold forceps. Right and left colon polyps had similar PT. Polyps < 10 mm had shorter PT than polyps ≥ 10 mm. There was no significant variability among five endoscopists; the PT of fellows was 0.3 minutes longer than attendings. The retrospective cohort included 1204 patients; 306 underwent colonoscopy after a positive mt-sDNA test and 898 underwent upfront colonoscopy. MIT was calculated using a median PT of 0.6 minutes. In the mt-sDNA group, the ADR for WT intervals of 6-9 minutes was 38% and 50% for 9-12 minutes. Using MIT, the ADR was better for interval 9-12 (61%). In the upfront colonoscopy cohort, MIT improved ADR compared to WT in both 6-9 (20% vs 23%) and 9-12 (42% vs 47%). Extending MIT to > 9 minutes resulted in a 73% (95% CI 1.29-2.32) greater likelihood to identify adenomas in the upfront cohort and a 37% improvement in ADR in the mt-sDNA cohort compared to 6-9 minutes.
Discussion: MIT as a quality indicator for colonoscopy provides a more accurate assessment of withdrawal time’s impact on ADR. Extending MIT beyond 9 minutes significantly enhances adenoma detection in upfront screening and diagnostic cohorts.
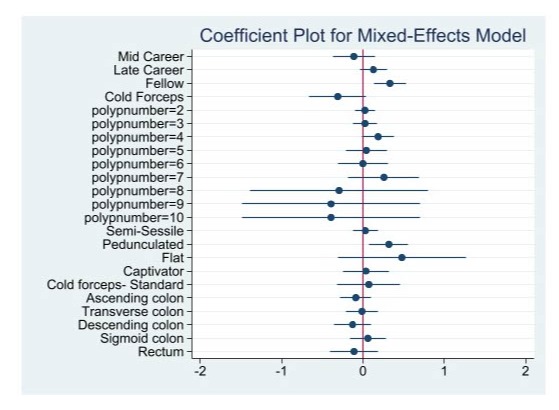
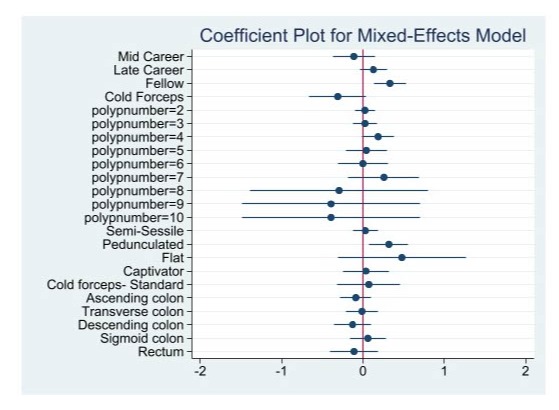
Figure: Image 1: Coefficient Regression Plot of Polypectomy Time.
Reference variables: Early career attending, Hot forceps, Polyp number 1 in same patient, Sessile polyps, Exacto snare, Cecum.
Reference variables: Early career attending, Hot forceps, Polyp number 1 in same patient, Sessile polyps, Exacto snare, Cecum.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Samuel Cheong indicated no relevant financial relationships.
Amar Vedamurthy indicated no relevant financial relationships.
Elise Le Cam indicated no relevant financial relationships.
Akira Folk indicated no relevant financial relationships.
Brendan Andres indicated no relevant financial relationships.
Malini Chauhan indicated no relevant financial relationships.
Shivanand Bomman indicated no relevant financial relationships.
Mahak Chauhan indicated no relevant financial relationships.
Avin Aggarwal indicated no relevant financial relationships.
Joshua Melson indicated no relevant financial relationships.
Samuel H. Cheong, DO1, Amar Vedamurthy, MD, MSCI, MRCP (UK)2, Elise Le Cam, MD1, Akira Folk, DO1, Brendan Andres, MD3, Malini Chauhan, MD4, Shivanand Bomman, MD4, Mahak Chauhan, MD1, Avin Aggarwal, MD5, Joshua Melson, MD4. P2135 - Measuring Mucosal Inspection Time to Determine Optimal Withdrawal Time in Diagnostic and Screening Colonoscopy: A Mixed Methods Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
