Monday Poster Session
Category: Endoscopy Video Forum
P2176 - A Knot So OK Pouch
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anusha Agarwal, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Roma Patel, MD1, Stephen Firkins, MD2, Anusha Agarwal, MD1, C Roberto Simon-Linares, MD2
1Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH
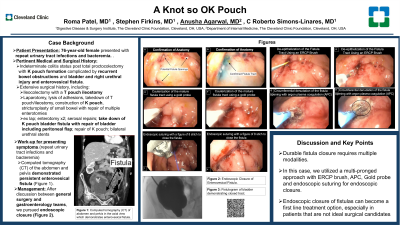
Introduction: The patient was a 76 year old woman with a past medical history significant for indeterminate colitis status post total proctocolectomy with K pouch formation in 2002 complicated by recurrent bowel obstructions requiring abdominal surgeries further complicated by bladder and right ureteral injury and enterovesical fistula. The patient has since undergone repair of the bladder fistula with takedown and revision of K pouch in 6/2023. She was admitted again for concern of recurrence of there enterovesical fistula.<br><br>The patient had undergone at least fourteen abdominal surgeries in her past with the most notable surgeries being the formation of the K pouch in 2002 and the most recent takedown of the K pouch, repair of the bladder fistula and reformation of the K pouch. In September of 2023 the patient presented with repeat urinary tract infections and bacteremia. Imaging showed persistent enterovesical fistula. After discussion between surgery and gastroenterology, attempt with endoscopic closure was attempted given patient’s frozen abdomen and comorbid conditions concerning for poor prognosis with surgery.
Case Description/Methods: Endoscopically, the anatomy of the K pouch was first appreciated through thorough exploration. The K pouch caused a natural retroflexion of the scope when the pouch was entered. The pouch was interrogated and areas that appeared suspicious for the fistula were identified. Then the patient’s bladder was filled with saline mixed with methylene blue and the location of the fistula was confirmed. A guide was then introduced with an endoscopic retrograde cholangiopancreatography brush to help de-epithelize the tract. Cauterization of the mature fistula tract using a gold probe helped promote fistula tract closure. Once the tract had been manipulated, the fistula opening was denuded in a circumferential patter with argon plasma coagulation and closed with endoscopic suturing in a figure of 8 stitch. The final endoscopic views did not show any visible fistula and repeat fistulograms over the next 3 weeks continued to confirm resolution.
Discussion: Endoscopic closure of fistulas is possible but there is currently no gold standard. As seen in this case, a multi-pronged method can be used to target these lesions and is very effective is keeping fistulas closed when both the tract and the opening are targeted. Endoscopic closure of fistulas can become a first line treatment option, especially in patients that are not ideal surgical candidates.
Disclosures:
Roma Patel, MD1, Stephen Firkins, MD2, Anusha Agarwal, MD1, C Roberto Simon-Linares, MD2. P2176 - A Knot So OK Pouch, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH
Introduction: The patient was a 76 year old woman with a past medical history significant for indeterminate colitis status post total proctocolectomy with K pouch formation in 2002 complicated by recurrent bowel obstructions requiring abdominal surgeries further complicated by bladder and right ureteral injury and enterovesical fistula. The patient has since undergone repair of the bladder fistula with takedown and revision of K pouch in 6/2023. She was admitted again for concern of recurrence of there enterovesical fistula.<br><br>The patient had undergone at least fourteen abdominal surgeries in her past with the most notable surgeries being the formation of the K pouch in 2002 and the most recent takedown of the K pouch, repair of the bladder fistula and reformation of the K pouch. In September of 2023 the patient presented with repeat urinary tract infections and bacteremia. Imaging showed persistent enterovesical fistula. After discussion between surgery and gastroenterology, attempt with endoscopic closure was attempted given patient’s frozen abdomen and comorbid conditions concerning for poor prognosis with surgery.
Case Description/Methods: Endoscopically, the anatomy of the K pouch was first appreciated through thorough exploration. The K pouch caused a natural retroflexion of the scope when the pouch was entered. The pouch was interrogated and areas that appeared suspicious for the fistula were identified. Then the patient’s bladder was filled with saline mixed with methylene blue and the location of the fistula was confirmed. A guide was then introduced with an endoscopic retrograde cholangiopancreatography brush to help de-epithelize the tract. Cauterization of the mature fistula tract using a gold probe helped promote fistula tract closure. Once the tract had been manipulated, the fistula opening was denuded in a circumferential patter with argon plasma coagulation and closed with endoscopic suturing in a figure of 8 stitch. The final endoscopic views did not show any visible fistula and repeat fistulograms over the next 3 weeks continued to confirm resolution.
Discussion: Endoscopic closure of fistulas is possible but there is currently no gold standard. As seen in this case, a multi-pronged method can be used to target these lesions and is very effective is keeping fistulas closed when both the tract and the opening are targeted. Endoscopic closure of fistulas can become a first line treatment option, especially in patients that are not ideal surgical candidates.
Disclosures:
Roma Patel indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Anusha Agarwal indicated no relevant financial relationships.
C Roberto Simon-Linares indicated no relevant financial relationships.
Roma Patel, MD1, Stephen Firkins, MD2, Anusha Agarwal, MD1, C Roberto Simon-Linares, MD2. P2176 - A Knot So OK Pouch, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
