Monday Poster Session
Category: Endoscopy Video Forum
P2180 - Electrosurgical Mucosotomy for Intramucosal Esophageal Dissection
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Scott MacKay, MD
University of Alberta
Edmonton, AB, Canada
Presenting Author(s)
Scott MacKay, MD1, John Yee, MD2, Ananya Nair, BSc3, Roberto Trasolini, MD2
1University of Alberta, Edmonton, AB, Canada; 2University of British Columbia, Vancouver, BC, Canada; 3University of Toronto, Toronto, ON, Canada
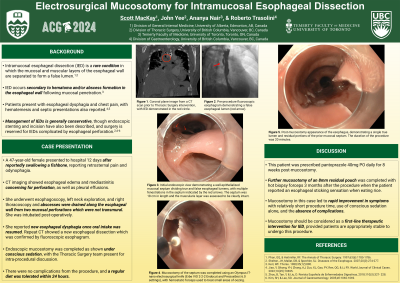
Introduction: Intramucosal esophageal dissection (IED) is a rare condition in which the mucosal and muscular layers of the esophageal wall are separated to form a false lumen. This separation occurs as a result of hematoma or abscess formation in the esophageal wall, which can occur spontaneously or following penetration of the esophageal mucosa. Management of IEDs is generally conservative, though endoscopic stenting and incision have been described in few case reports to date. In the current case, endoscopic electrosurgical mucosotomy was utilized for IED at the time of diagnosis.
Case Description/Methods: A 47-year-old woman presented to hospital with retrosternal pleuritic chest pain and odynophagia after reportedly swallowing a fishbone 12 days earlier. Thoracic Surgery performed an urgent esophagoscopy for drainage of prevertebral and mediastinal collections, with 2 discrete perforations that were not transmural observed intra-operatively. The patient was intubated post-operatively and, after eventual extubation, reported new esophageal dysphagia. A fluoroscopic esophagram demonstrated a new false esophageal lumen. Esophagogastroduodenoscopy was completed on post-operative day 44 and a large mucosal septum with multiple small fenestrations between the true and false esophageal lumens was identified. This appearance was in keeping with an IED that was eighteen centimetres in length, with the muscularis layer visible and intact. An electrosurgical knife was used to completed a mucosotomy along the length of the septum and transection of several small bridges of musical tissue to deroof the clean and well-epithelialized cavity. Small areas of oozing on the transected flap were treated with hemostatic forceps and the esophagus was left to heal via secondary intention. The patient reported immediate improvement in esophageal dysphagia and was able to tolerate a regular diet within 24 hours of this procedure.
Discussion: This case demonstrates the utility of mucosotomy in IED as evidenced by the rapid improvement in symptoms reported by the patient and the absence of procedural complications. While rare, patients who present with IED often undergo endoscopy and endoscopic mucosotomy should be considered as a first-line therapeutic intervention provided patients are appropriately stable to undergo this procedure.
Disclosures:
Scott MacKay, MD1, John Yee, MD2, Ananya Nair, BSc3, Roberto Trasolini, MD2. P2180 - Electrosurgical Mucosotomy for Intramucosal Esophageal Dissection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alberta, Edmonton, AB, Canada; 2University of British Columbia, Vancouver, BC, Canada; 3University of Toronto, Toronto, ON, Canada
Introduction: Intramucosal esophageal dissection (IED) is a rare condition in which the mucosal and muscular layers of the esophageal wall are separated to form a false lumen. This separation occurs as a result of hematoma or abscess formation in the esophageal wall, which can occur spontaneously or following penetration of the esophageal mucosa. Management of IEDs is generally conservative, though endoscopic stenting and incision have been described in few case reports to date. In the current case, endoscopic electrosurgical mucosotomy was utilized for IED at the time of diagnosis.
Case Description/Methods: A 47-year-old woman presented to hospital with retrosternal pleuritic chest pain and odynophagia after reportedly swallowing a fishbone 12 days earlier. Thoracic Surgery performed an urgent esophagoscopy for drainage of prevertebral and mediastinal collections, with 2 discrete perforations that were not transmural observed intra-operatively. The patient was intubated post-operatively and, after eventual extubation, reported new esophageal dysphagia. A fluoroscopic esophagram demonstrated a new false esophageal lumen. Esophagogastroduodenoscopy was completed on post-operative day 44 and a large mucosal septum with multiple small fenestrations between the true and false esophageal lumens was identified. This appearance was in keeping with an IED that was eighteen centimetres in length, with the muscularis layer visible and intact. An electrosurgical knife was used to completed a mucosotomy along the length of the septum and transection of several small bridges of musical tissue to deroof the clean and well-epithelialized cavity. Small areas of oozing on the transected flap were treated with hemostatic forceps and the esophagus was left to heal via secondary intention. The patient reported immediate improvement in esophageal dysphagia and was able to tolerate a regular diet within 24 hours of this procedure.
Discussion: This case demonstrates the utility of mucosotomy in IED as evidenced by the rapid improvement in symptoms reported by the patient and the absence of procedural complications. While rare, patients who present with IED often undergo endoscopy and endoscopic mucosotomy should be considered as a first-line therapeutic intervention provided patients are appropriately stable to undergo this procedure.
Disclosures:
Scott MacKay indicated no relevant financial relationships.
John Yee indicated no relevant financial relationships.
Ananya Nair indicated no relevant financial relationships.
Roberto Trasolini: Boston Scientific – Consultant. Fractyl Health – Consultant. Fujifilm – Consultant. Medtronic – Consultant.
Scott MacKay, MD1, John Yee, MD2, Ananya Nair, BSc3, Roberto Trasolini, MD2. P2180 - Electrosurgical Mucosotomy for Intramucosal Esophageal Dissection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
