Monday Poster Session
Category: Esophagus
P2203 - FLIP Measurements and Opening Classifications After Pneumatic Dilation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

James Miller, MD
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
James Miller, MD, Steven Clayton, MD
Wake Forest University School of Medicine, Winston-Salem, NC
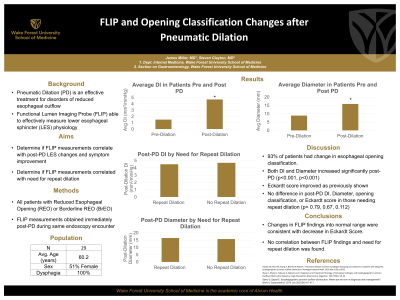
Introduction: Pneumatic dilation (PD) has been shown to be an effective treatment for disorders of reduced esophageal opening with improvement in symptoms. Functional Lumen Impedance Planimetry (FLIP) can effectively measure lower esophageal sphincter (LES) physiology compared to esophageal standards. The aim of this analysis was to evaluate if FLIP measurements and esophageal opening classifications changed consistently with symptom improvement post-PD. Also, to determine if post-PD FLIP measurement correlated with need for repeat dilation.
Methods: FLIP data from endoscopy procedure notes and subjective symptom scores from clinic follow up encounters were obtained through chart review. Post-PD FLIP measurements were taken immediately after PD during the same endoscopy encounter. Repeat dilations were performed with a 35mm balloon.
Results: A total of 29 patients with Reduced Esophageal Opening (REO) or Borderline REO (BrEO) pre-PD were included in the analysis. 27 patients (93%) had improved opening classification to normal (NEO) or borderline normal (BnEO) immediately after PD.
After PD, average Distensibility Index (DI) increased from 1.5 mm2/mmHg to 4.7 mm2/mmHg (p< 0.001) and diameter changed from 8.9 mm to 15.9 mm (p< 0.001).
15 patients had Eckardt Score documented at their 6-8 week follow up appointment. Average post-dilation Eckardt score was 1.2, decreased from average pre-dilation score of 6.25.
6 patients underwent repeat dilation with average interval of 17.8 months. 67% underwent repeat PD. Of those that required repeat dilations, average post-dilation DI was 4.5 mm2/mmHg and diameter 16.4 mm, not statistically different than those that did not undergo repeat procedure (4.7 mm2/mmHg, 15.7 mm p= 0.79, 0.67 respectively). Post-dilation esophageal opening were all NEO or BnEO. Pre-dilation opening criteria all changed post-dilation, 67% of which were REO. Average Eckardt score at 6-8 week follow up for these patients was 1.4, not significantly different than those who did not require repeat dilation (0.7, p=0.112).
Discussion: PD appears to be associated with improved esophageal opening classification and significant change in both DI and diameter, consistent with improved Eckardt score. Post-dilation DI, diameter, esophageal opening pattern, and Eckardt score were not indicative of need for repeat dilation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
James Miller, MD, Steven Clayton, MD. P2203 - FLIP Measurements and Opening Classifications After Pneumatic Dilation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Pneumatic dilation (PD) has been shown to be an effective treatment for disorders of reduced esophageal opening with improvement in symptoms. Functional Lumen Impedance Planimetry (FLIP) can effectively measure lower esophageal sphincter (LES) physiology compared to esophageal standards. The aim of this analysis was to evaluate if FLIP measurements and esophageal opening classifications changed consistently with symptom improvement post-PD. Also, to determine if post-PD FLIP measurement correlated with need for repeat dilation.
Methods: FLIP data from endoscopy procedure notes and subjective symptom scores from clinic follow up encounters were obtained through chart review. Post-PD FLIP measurements were taken immediately after PD during the same endoscopy encounter. Repeat dilations were performed with a 35mm balloon.
Results: A total of 29 patients with Reduced Esophageal Opening (REO) or Borderline REO (BrEO) pre-PD were included in the analysis. 27 patients (93%) had improved opening classification to normal (NEO) or borderline normal (BnEO) immediately after PD.
After PD, average Distensibility Index (DI) increased from 1.5 mm2/mmHg to 4.7 mm2/mmHg (p< 0.001) and diameter changed from 8.9 mm to 15.9 mm (p< 0.001).
15 patients had Eckardt Score documented at their 6-8 week follow up appointment. Average post-dilation Eckardt score was 1.2, decreased from average pre-dilation score of 6.25.
6 patients underwent repeat dilation with average interval of 17.8 months. 67% underwent repeat PD. Of those that required repeat dilations, average post-dilation DI was 4.5 mm2/mmHg and diameter 16.4 mm, not statistically different than those that did not undergo repeat procedure (4.7 mm2/mmHg, 15.7 mm p= 0.79, 0.67 respectively). Post-dilation esophageal opening were all NEO or BnEO. Pre-dilation opening criteria all changed post-dilation, 67% of which were REO. Average Eckardt score at 6-8 week follow up for these patients was 1.4, not significantly different than those who did not require repeat dilation (0.7, p=0.112).
Discussion: PD appears to be associated with improved esophageal opening classification and significant change in both DI and diameter, consistent with improved Eckardt score. Post-dilation DI, diameter, esophageal opening pattern, and Eckardt score were not indicative of need for repeat dilation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
James Miller indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
James Miller, MD, Steven Clayton, MD. P2203 - FLIP Measurements and Opening Classifications After Pneumatic Dilation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
