Monday Poster Session
Category: Esophagus
P2221 - Mean Nocturnal Baseline Impedance is Lower in Patients With Erosive Reflux Disease, Barrett’s Esophagus, Higher Body Mass Index, in Comparison With Nonerosive Reflux Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chaewon Jeong, BS
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Chaewon Jeong, BS, Bailey C. McCollum, BA, Steven Clayton, MD
Wake Forest University School of Medicine, Winston-Salem, NC
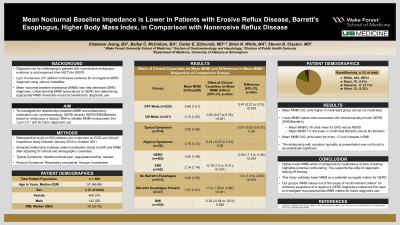
Introduction: The Lyon Consensus 2.01 has defined conclusive evidence for gastroesophageal reflux disease (GERD) through various modalities; however, diagnosis can be challenging in patients with inconclusive endoscopic evidence or acid exposure time (AET). Mean nocturnal baseline impedance (MNBI) is a novel metric developed to help delineate pathological GERD. Our study aimed to investigate the relationships between MNBI, GERD (characterized as nonerosive (NERD)/erosive reflux disease (ERD)/Barrett’s esophagus via biopsy) by endoscopy, and common factors such as antisecretory medication use and symptomatology to further validate MNBI incorporation into Lyon 2.0.
Methods: We performed a retrospective study on 550 patients who underwent an EGD and 24h-pH Impedance study. A multivariate linear mixed model was used to infer the relationship between patient medication status (on/off) and MNBI after adjusting for clinical and demographic covariates. Interaction terms determined whether effect of patient medication status on MNBI was moderated by other clinical covariates. Analyses performed in R v.4.1.1.
Results: Interaction terms suggested that the effect of medication status on MNBI is independent of the clinical covariates. The main effects model inferred that medication status, endoscopic evidence of NERD/ERD/Barrett’s, and BMI had statistically significant independent effects on MNBI (Table 1). The mean MNBI (kOhm) was 0.52 units higher (95% CI: 0.27, 7.8; p< 0.001) in medicated patients compared to those not medicated. Patients with ERD had a mean MNBI 0.78 units lower (95% CI: -1.2, -0.41; p< 0.001) than those with NERD. Patients with Barrett’s had a mean MNBI decrease of 1 unit (95% CI: -1.5, -0.5; p< 0.001) compared to non-Barrett’s patients. Also, for every 1.0 unit increase in BMI the mean MNBI decreased 0.02 (95% CI: -0.04, -0.01; p=0.006) units.
Discussion: Our large study findings corroborate Lyon 2.0 in that lower MNBI ranges were associated with endoscopically proven GERD, namely, ERD and Barrett’s. The results of this study validate lower MNBI as a surrogate marker for GERD. Additionally, increased mean MNBI of patients on antisecretory medications compared to those off medication at time of pH testing highlights the significance of medication use during studies as a potential confounding factor, and supports the utility of testing off therapy.
1Gyawali, et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0, Jan 5, 2024; 361-371
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chaewon Jeong, BS, Bailey C. McCollum, BA, Steven Clayton, MD. P2221 - Mean Nocturnal Baseline Impedance is Lower in Patients With Erosive Reflux Disease, Barrett’s Esophagus, Higher Body Mass Index, in Comparison With Nonerosive Reflux Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: The Lyon Consensus 2.01 has defined conclusive evidence for gastroesophageal reflux disease (GERD) through various modalities; however, diagnosis can be challenging in patients with inconclusive endoscopic evidence or acid exposure time (AET). Mean nocturnal baseline impedance (MNBI) is a novel metric developed to help delineate pathological GERD. Our study aimed to investigate the relationships between MNBI, GERD (characterized as nonerosive (NERD)/erosive reflux disease (ERD)/Barrett’s esophagus via biopsy) by endoscopy, and common factors such as antisecretory medication use and symptomatology to further validate MNBI incorporation into Lyon 2.0.
Methods: We performed a retrospective study on 550 patients who underwent an EGD and 24h-pH Impedance study. A multivariate linear mixed model was used to infer the relationship between patient medication status (on/off) and MNBI after adjusting for clinical and demographic covariates. Interaction terms determined whether effect of patient medication status on MNBI was moderated by other clinical covariates. Analyses performed in R v.4.1.1.
Results: Interaction terms suggested that the effect of medication status on MNBI is independent of the clinical covariates. The main effects model inferred that medication status, endoscopic evidence of NERD/ERD/Barrett’s, and BMI had statistically significant independent effects on MNBI (Table 1). The mean MNBI (kOhm) was 0.52 units higher (95% CI: 0.27, 7.8; p< 0.001) in medicated patients compared to those not medicated. Patients with ERD had a mean MNBI 0.78 units lower (95% CI: -1.2, -0.41; p< 0.001) than those with NERD. Patients with Barrett’s had a mean MNBI decrease of 1 unit (95% CI: -1.5, -0.5; p< 0.001) compared to non-Barrett’s patients. Also, for every 1.0 unit increase in BMI the mean MNBI decreased 0.02 (95% CI: -0.04, -0.01; p=0.006) units.
Discussion: Our large study findings corroborate Lyon 2.0 in that lower MNBI ranges were associated with endoscopically proven GERD, namely, ERD and Barrett’s. The results of this study validate lower MNBI as a surrogate marker for GERD. Additionally, increased mean MNBI of patients on antisecretory medications compared to those off medication at time of pH testing highlights the significance of medication use during studies as a potential confounding factor, and supports the utility of testing off therapy.
1Gyawali, et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0, Jan 5, 2024; 361-371
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Chaewon Jeong indicated no relevant financial relationships.
Bailey McCollum indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Chaewon Jeong, BS, Bailey C. McCollum, BA, Steven Clayton, MD. P2221 - Mean Nocturnal Baseline Impedance is Lower in Patients With Erosive Reflux Disease, Barrett’s Esophagus, Higher Body Mass Index, in Comparison With Nonerosive Reflux Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

