Monday Poster Session
Category: Esophagus
P2223 - Overutilization of Proton Pump Inhibitors in a Community-Based Hospital: A QI Initiative
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- TN
Tripti Nagar, MD
Wayne State University School of Medicine
Rochester, MI
Presenting Author(s)
Tripti Nagar, MD1, Alaa Taha, MD2, Anthony Calabrese, MD1, Ayushi Garg, MD1, Vesna Tegeltija, MD1
1Wayne State University School of Medicine, Rochester, MI; 2Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Rochester, MI
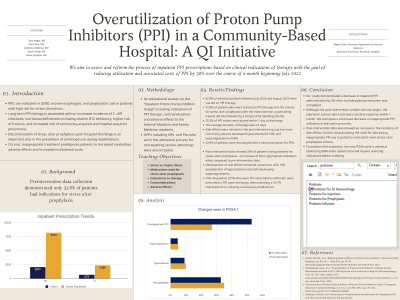
Introduction: Inpatient proton pump inhibitors (PPIs) are used for acid-producing pathologies and prophylactically for stress ulceration prevention in those with risk factors. Long-term therapy is associated with an increased incidence of infections, nutritional deficiencies including B12 deficiency, and a higher risk of fractures. Discontinuation of prophylactic PPIs upon hospital discharge is an important step in preventing unnecessary PPI use, particularly in the event of readmission. With this quality improvement (QI) initiative, we aim to reform the process of inpatient PPI orders to reduce inappropriate utilization by 30% over 6 months, beginning July 2022.
Methods: Pre-intervention data was collected between July and August 2022. Descriptive analysis showed overutilization among all inpatient admissions, including the teaching services. Root cause analysis revealed a lack of knowledge regarding PPI indications and adverse effects. A Plan-Do-Study-Act (PDSA) cycle was used to test change. An educational session was conducted in April 2023 to all teaching services and admitting advanced practice providers (APPs). This presentation reviewed indications for therapy, stress ulcers vs. peptic ulcer development, medications used, contraindications, and adverse effects.
Results: 50.5% of the pre-intervention patients had a prior diagnosis justifying inpatient PPI usage. 83.8% of all patients were started on PPI therapy upon admission, however, 25.2% of orders were placed within one day of discharge. The most common side effects included hypocalcemia (9.13%) and hypomagnesemia (4.8%). 52.9% of patients were discharged with a new PPI prescription.
Post-intervention data from May to August 2023 showed 56% of patients had a pre-existing diagnosis for resumption of PPIs. Of the remaining patients, 35% met stress ulcer prophylaxis criteria. This was a 3% increase in appropriate utilization. Side effects remained uncommon, seen in 24.4% of the total cohort. 27% of patients were discharged with a new PPI prescription.
Discussion: Our data supports existing data that PPIs are well-tolerated, however, they are not without risk, particularly in patients with cardiac or renal comorbidities. Post-intervention, a 3% increase in appropriate utilization was seen. Our intervention did reduce the number of PPI-naive patients who were discharged with PPIs by 25.7%. To maintain this trajectory, our next PDSA cycle optimizes the EMR order options requiring indication selection.
Disclosures:
Tripti Nagar, MD1, Alaa Taha, MD2, Anthony Calabrese, MD1, Ayushi Garg, MD1, Vesna Tegeltija, MD1. P2223 - Overutilization of Proton Pump Inhibitors in a Community-Based Hospital: A QI Initiative, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine, Rochester, MI; 2Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Rochester, MI
Introduction: Inpatient proton pump inhibitors (PPIs) are used for acid-producing pathologies and prophylactically for stress ulceration prevention in those with risk factors. Long-term therapy is associated with an increased incidence of infections, nutritional deficiencies including B12 deficiency, and a higher risk of fractures. Discontinuation of prophylactic PPIs upon hospital discharge is an important step in preventing unnecessary PPI use, particularly in the event of readmission. With this quality improvement (QI) initiative, we aim to reform the process of inpatient PPI orders to reduce inappropriate utilization by 30% over 6 months, beginning July 2022.
Methods: Pre-intervention data was collected between July and August 2022. Descriptive analysis showed overutilization among all inpatient admissions, including the teaching services. Root cause analysis revealed a lack of knowledge regarding PPI indications and adverse effects. A Plan-Do-Study-Act (PDSA) cycle was used to test change. An educational session was conducted in April 2023 to all teaching services and admitting advanced practice providers (APPs). This presentation reviewed indications for therapy, stress ulcers vs. peptic ulcer development, medications used, contraindications, and adverse effects.
Results: 50.5% of the pre-intervention patients had a prior diagnosis justifying inpatient PPI usage. 83.8% of all patients were started on PPI therapy upon admission, however, 25.2% of orders were placed within one day of discharge. The most common side effects included hypocalcemia (9.13%) and hypomagnesemia (4.8%). 52.9% of patients were discharged with a new PPI prescription.
Post-intervention data from May to August 2023 showed 56% of patients had a pre-existing diagnosis for resumption of PPIs. Of the remaining patients, 35% met stress ulcer prophylaxis criteria. This was a 3% increase in appropriate utilization. Side effects remained uncommon, seen in 24.4% of the total cohort. 27% of patients were discharged with a new PPI prescription.
Discussion: Our data supports existing data that PPIs are well-tolerated, however, they are not without risk, particularly in patients with cardiac or renal comorbidities. Post-intervention, a 3% increase in appropriate utilization was seen. Our intervention did reduce the number of PPI-naive patients who were discharged with PPIs by 25.7%. To maintain this trajectory, our next PDSA cycle optimizes the EMR order options requiring indication selection.
Disclosures:
Tripti Nagar indicated no relevant financial relationships.
Alaa Taha indicated no relevant financial relationships.
Anthony Calabrese indicated no relevant financial relationships.
Ayushi Garg indicated no relevant financial relationships.
Vesna Tegeltija indicated no relevant financial relationships.
Tripti Nagar, MD1, Alaa Taha, MD2, Anthony Calabrese, MD1, Ayushi Garg, MD1, Vesna Tegeltija, MD1. P2223 - Overutilization of Proton Pump Inhibitors in a Community-Based Hospital: A QI Initiative, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
