Monday Poster Session
Category: Esophagus
P2257 - Incidental Finding of Esophageal Intramural Diverticulosis in Elderly Male With Recurrent Dysphagia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Juan Cerezo, MD
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Juan Cerezo, MD, Gabriel Castillo, MD, Rabia De Latour, MD
NYU Grossman School of Medicine, New York, NY
Introduction: Esophageal intramural pseudodiverticulosis (EIP) is a rare cause of dysphagia that is characterized by multiple small flask-shaped outpouchings of the esophageal wall. These outpouchings are thought to be due to localized inflammation of the esophagus that causes mucosal gland hypertrophy, creating cystic-like cavities that can be seen on endoscopy. Esophageal strictures can result from chronic inflammation. We present a case of a patient with recurrent dysphagia found to have EIP complicated by severe esophageal stenosis.
Case Description/Methods:
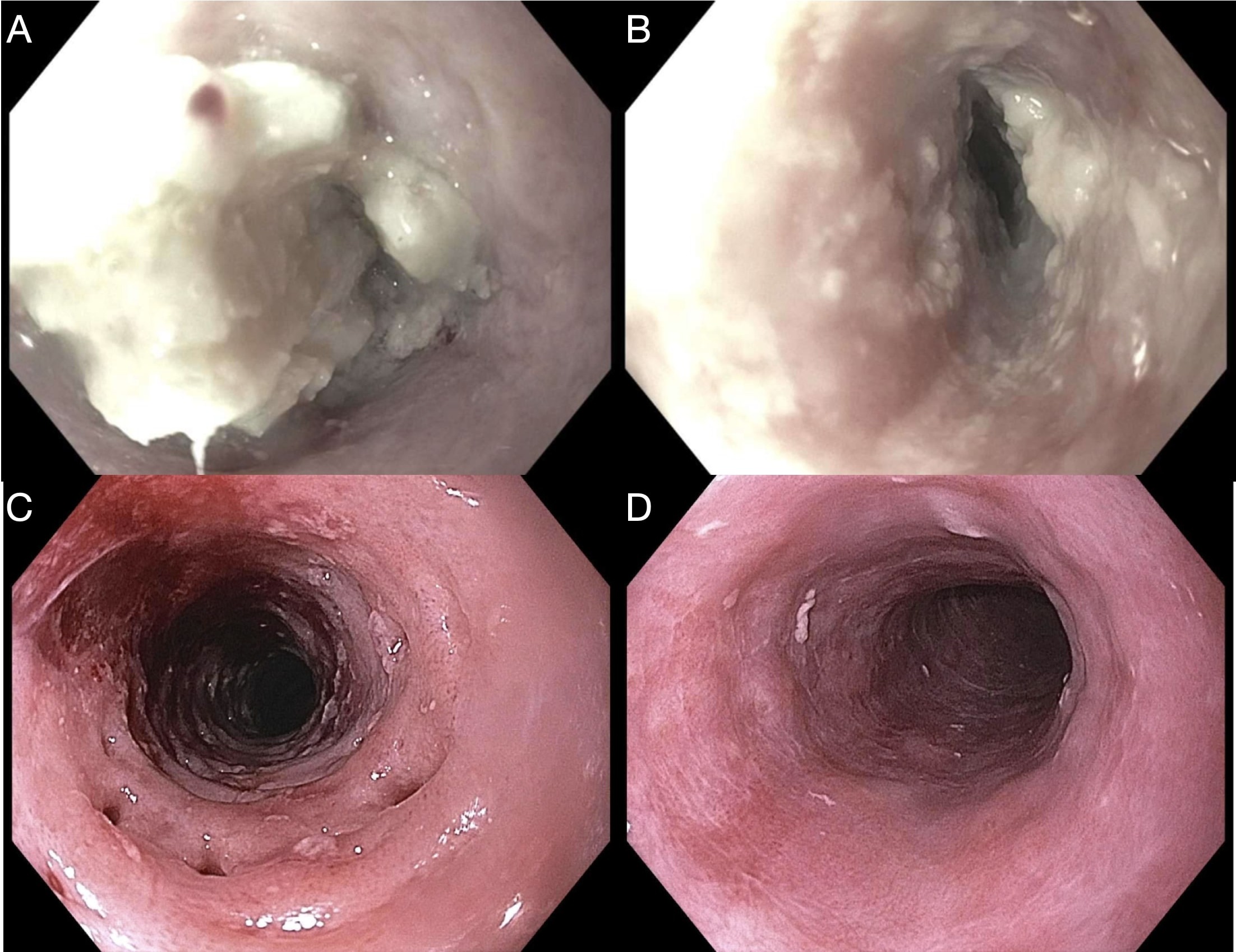
A 71-year-old male with previously diagnosed esophageal stenosis treated with balloon dilation presented with an inability to swallow and neck discomfort after consuming a meal. His blood pressure was 155/76 but other vital signs were within normal limits. Flexible laryngoscopy revealed a clear upper away. Endoscopy revealed LA Grade D esophagitis with friable mucosa and food impaction. The gastroesophageal junction was visible after food retrieval, but endoscope could not be advanced due to the degree of stenosis.
Repeat endoscopy 2 months later revealed moderate stenosis that was traversed and dilated using the endoscope. Mucosal erythema with small outpouchings were seen in the upper third of the esophagus. Mild erythema was present in the lower two thirds of the esophagus. Biopsies were taken of the entire esophagus. The stomach and proximal duodenum were normal, and no further dilation was performed. Histology showed active esophagitis with intraepithelial lymphocytes. Testing for candidiasis, CMV and HSV was negative.
Discussion: EIP is associated with diabetes, esophageal candidiasis, gastroesophageal reflux disease, and chronic alcohol and tobacco use. It is often found late in the disease course after the inflammation has begun causing symptoms of dysphagia. In severe cases, esophageal stenosis can cause food bolus impaction.
Histopathology can show inflammatory cell infiltration, epithelial and basal cell hyperplasia, thickening of the ductal wall, and preservation of the acinar cells in the submucosa. However, endoscopic biopsies commonly show nonspecific inflammation as the pseudodiverticula lie intramurally and may not be included in biopsied samples. EIP is symptomatically managed with esophageal dilation. Treatment of concomitant reflux esophagitis or candidiasis have also been reported to reduce inflammation and relieve symptoms. The patient’s symptoms improved after dilation and was recommended continued follow-up.
Disclosures:
Juan Cerezo, MD, Gabriel Castillo, MD, Rabia De Latour, MD. P2257 - Incidental Finding of Esophageal Intramural Diverticulosis in Elderly Male With Recurrent Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYU Grossman School of Medicine, New York, NY
Introduction: Esophageal intramural pseudodiverticulosis (EIP) is a rare cause of dysphagia that is characterized by multiple small flask-shaped outpouchings of the esophageal wall. These outpouchings are thought to be due to localized inflammation of the esophagus that causes mucosal gland hypertrophy, creating cystic-like cavities that can be seen on endoscopy. Esophageal strictures can result from chronic inflammation. We present a case of a patient with recurrent dysphagia found to have EIP complicated by severe esophageal stenosis.
Case Description/Methods:
A 71-year-old male with previously diagnosed esophageal stenosis treated with balloon dilation presented with an inability to swallow and neck discomfort after consuming a meal. His blood pressure was 155/76 but other vital signs were within normal limits. Flexible laryngoscopy revealed a clear upper away. Endoscopy revealed LA Grade D esophagitis with friable mucosa and food impaction. The gastroesophageal junction was visible after food retrieval, but endoscope could not be advanced due to the degree of stenosis.
Repeat endoscopy 2 months later revealed moderate stenosis that was traversed and dilated using the endoscope. Mucosal erythema with small outpouchings were seen in the upper third of the esophagus. Mild erythema was present in the lower two thirds of the esophagus. Biopsies were taken of the entire esophagus. The stomach and proximal duodenum were normal, and no further dilation was performed. Histology showed active esophagitis with intraepithelial lymphocytes. Testing for candidiasis, CMV and HSV was negative.
Discussion: EIP is associated with diabetes, esophageal candidiasis, gastroesophageal reflux disease, and chronic alcohol and tobacco use. It is often found late in the disease course after the inflammation has begun causing symptoms of dysphagia. In severe cases, esophageal stenosis can cause food bolus impaction.
Histopathology can show inflammatory cell infiltration, epithelial and basal cell hyperplasia, thickening of the ductal wall, and preservation of the acinar cells in the submucosa. However, endoscopic biopsies commonly show nonspecific inflammation as the pseudodiverticula lie intramurally and may not be included in biopsied samples. EIP is symptomatically managed with esophageal dilation. Treatment of concomitant reflux esophagitis or candidiasis have also been reported to reduce inflammation and relieve symptoms. The patient’s symptoms improved after dilation and was recommended continued follow-up.
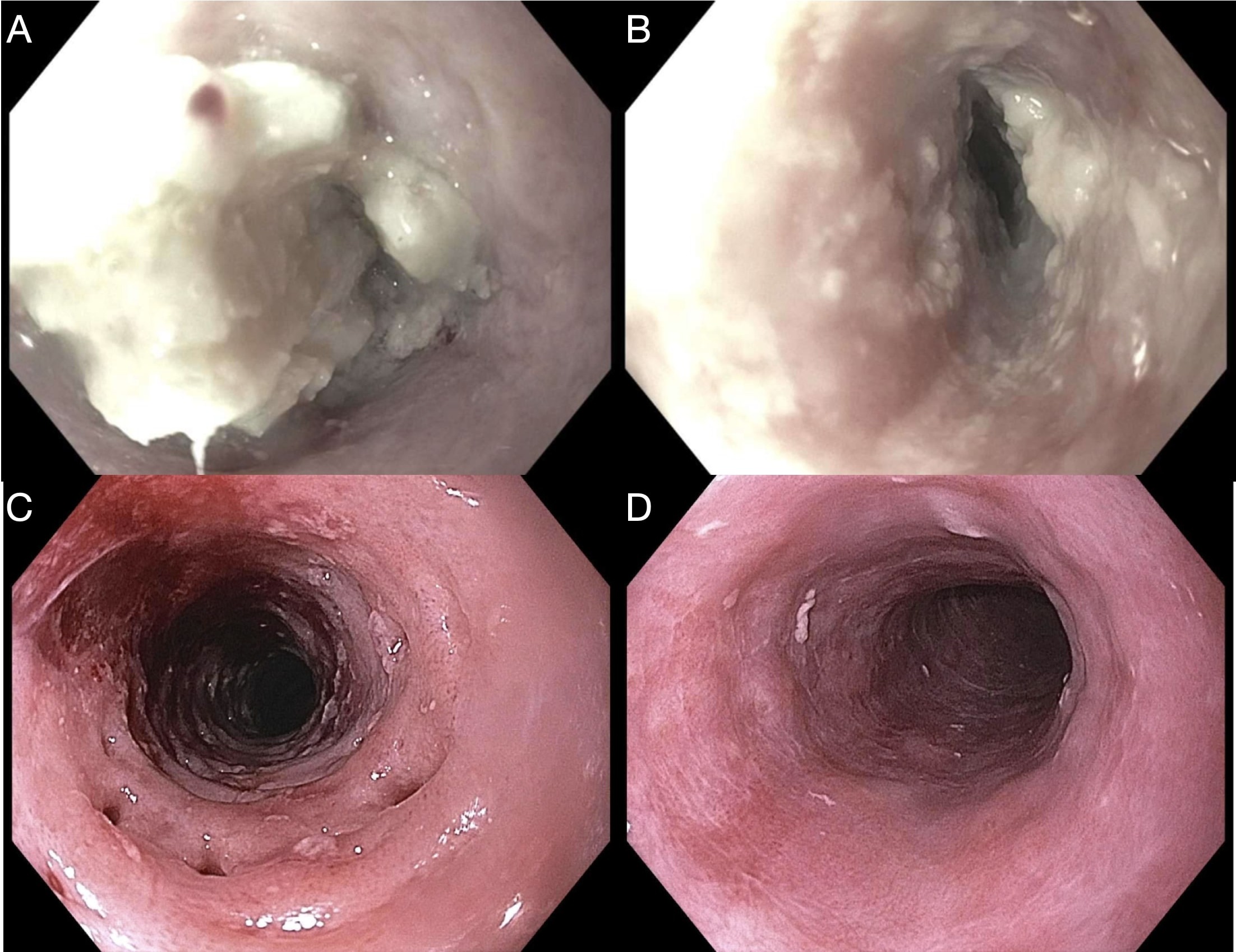
Figure: Initial EGD showing esophagus with food impaction (A) and esophageal stenosis seen after removal of food bolus (B). Follow up EGD revealing outpouchings (C) and mucosal erythema in the middle third of esophagus (D).
Disclosures:
Juan Cerezo indicated no relevant financial relationships.
Gabriel Castillo indicated no relevant financial relationships.
Rabia De Latour: Boston Sci – Speakers Bureau.
Juan Cerezo, MD, Gabriel Castillo, MD, Rabia De Latour, MD. P2257 - Incidental Finding of Esophageal Intramural Diverticulosis in Elderly Male With Recurrent Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
