Monday Poster Session
Category: Esophagus
P2258 - Rapidly Growing Adenocarcinoma at the Gastroesophageal Junction 18 Years After Roux-en-Y Gastric Bypass: A Case Report and Review of Surveillance Necessities
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jaskaranpreet Kaur, MD, MS
North Alabama Medical Center
Florence, AL
Presenting Author(s)
Jaskaranpreet Kaur, MD, MS1, Navneet Kaur, MD1, Sheena Bhushan, MD2, Barath Prashanth Sivasubramanian, MD2
1North Alabama Medical Center, Florence, AL; 2Northeast Georgia Medical Center, Gainesville, GA
Introduction: Bariatric surgery, a rapidly growing operative procedure, had over 579,000 procedures performed in 2014. There is still a debate regarding whether bariatric surgery increases the risk of esophagus or stomach malignancy. We want to highlight the case of a 69-year-old patient who developed rapidly growing poorly differentiated adenocarcinoma at the gastroesophageal (GE) junction 18 years after Roux-en-Y gastric bypass (RYGB) surgery. This cancer developed within three months.
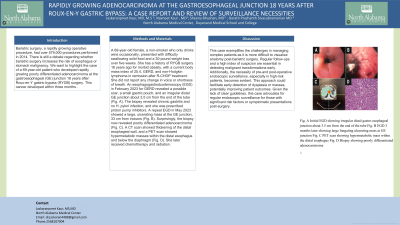
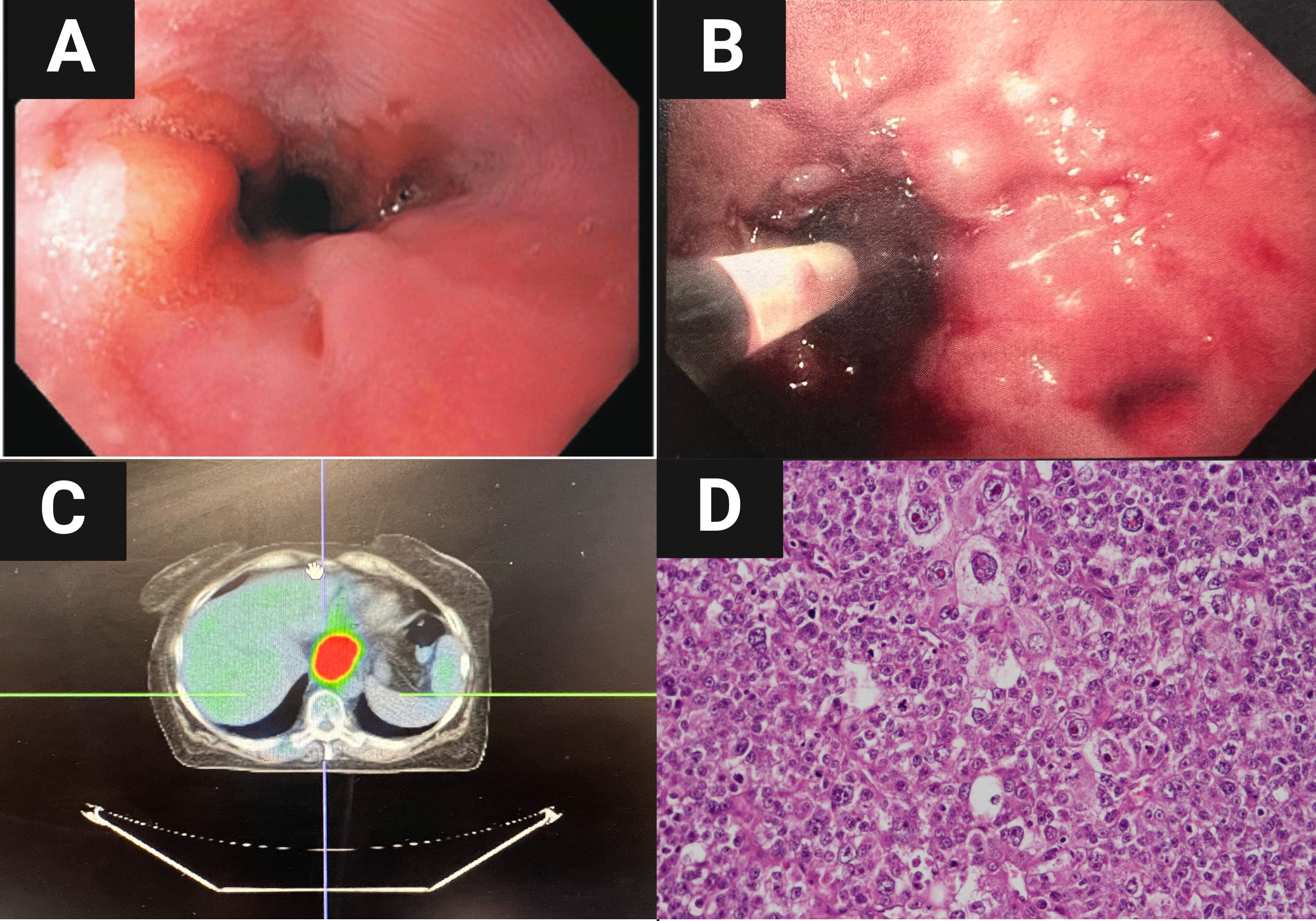
Case Description/Methods: A 69-year-old female, a non-smoker who only drinks wine occasionally, presented with difficulty swallowing solid food and a 30-pound weight loss over five weeks. She has a history of RYGB surgery 18 years ago for morbid obesity, with a current body mass index of 25.4, GERD, and non-Hodgkin lymphoma in remission after R-CHOP treatment. She did not report any change in voice or shortness of breath. An esophagogastroduodenoscopy (EGD) in February 2023 for GERD revealed a possible scar, a small gastric pouch, and an irregular distal GE junction about 3.5 cm from the end of the tube (Fig. A). The biopsy revealed chronic gastritis and no H. pylori infection, and she was prescribed proton pump inhibitors. A repeat EGD in May 2023 showed a large, ulcerating mass at the GE junction, 33 cm from incisors (Fig. B). Surprisingly, the biopsy now revealed poorly differentiated adenocarcinoma (Fig. C). A CT scan showed thickening of the distal esophageal wall, and a PET scan showed hypermetabolic masses within the distal esophagus and below the diaphragm (Fig. D). She later received chemotherapy and radiation.
Discussion: This case exemplifies the challenges in managing complex patients as it is more difficult to visualize anatomy post-bariatric surgery. Regular follow-ups and a high index of suspicion are essential in detecting malignant transformations early. Additionally, the necessity of pre-and post-operative endoscopic surveillance, especially in high-risk patients, becomes evident. This approach could facilitate early detection of dysplasia or masses, potentially improving patient outcomes. Given the lack of clear guidelines, this case advocates for regular endoscopic surveillance for those with significant risk factors or symptomatic presentations post-surgery.
Disclosures:
Jaskaranpreet Kaur, MD, MS1, Navneet Kaur, MD1, Sheena Bhushan, MD2, Barath Prashanth Sivasubramanian, MD2. P2258 - Rapidly Growing Adenocarcinoma at the Gastroesophageal Junction 18 Years After Roux-en-Y Gastric Bypass: A Case Report and Review of Surveillance Necessities, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1North Alabama Medical Center, Florence, AL; 2Northeast Georgia Medical Center, Gainesville, GA
Introduction: Bariatric surgery, a rapidly growing operative procedure, had over 579,000 procedures performed in 2014. There is still a debate regarding whether bariatric surgery increases the risk of esophagus or stomach malignancy. We want to highlight the case of a 69-year-old patient who developed rapidly growing poorly differentiated adenocarcinoma at the gastroesophageal (GE) junction 18 years after Roux-en-Y gastric bypass (RYGB) surgery. This cancer developed within three months.
Case Description/Methods: A 69-year-old female, a non-smoker who only drinks wine occasionally, presented with difficulty swallowing solid food and a 30-pound weight loss over five weeks. She has a history of RYGB surgery 18 years ago for morbid obesity, with a current body mass index of 25.4, GERD, and non-Hodgkin lymphoma in remission after R-CHOP treatment. She did not report any change in voice or shortness of breath. An esophagogastroduodenoscopy (EGD) in February 2023 for GERD revealed a possible scar, a small gastric pouch, and an irregular distal GE junction about 3.5 cm from the end of the tube (Fig. A). The biopsy revealed chronic gastritis and no H. pylori infection, and she was prescribed proton pump inhibitors. A repeat EGD in May 2023 showed a large, ulcerating mass at the GE junction, 33 cm from incisors (Fig. B). Surprisingly, the biopsy now revealed poorly differentiated adenocarcinoma (Fig. C). A CT scan showed thickening of the distal esophageal wall, and a PET scan showed hypermetabolic masses within the distal esophagus and below the diaphragm (Fig. D). She later received chemotherapy and radiation.
Discussion: This case exemplifies the challenges in managing complex patients as it is more difficult to visualize anatomy post-bariatric surgery. Regular follow-ups and a high index of suspicion are essential in detecting malignant transformations early. Additionally, the necessity of pre-and post-operative endoscopic surveillance, especially in high-risk patients, becomes evident. This approach could facilitate early detection of dysplasia or masses, potentially improving patient outcomes. Given the lack of clear guidelines, this case advocates for regular endoscopic surveillance for those with significant risk factors or symptomatic presentations post-surgery.
Figure: Fig. A Initial EGD showing irregular distal gastro-esophageal junction about 3.5 cm from the end of the tube
Fig. B EGD 3 months later showing large fungating ulcerating mass at GE junction
Fig. C PET scan showing hypermetabolic mass within the distal esophagus
Fig. D Biopsy showing poorly differentiated adenocarcinoma
Fig. B EGD 3 months later showing large fungating ulcerating mass at GE junction
Fig. C PET scan showing hypermetabolic mass within the distal esophagus
Fig. D Biopsy showing poorly differentiated adenocarcinoma
Disclosures:
Jaskaranpreet Kaur indicated no relevant financial relationships.
Navneet Kaur indicated no relevant financial relationships.
Sheena Bhushan indicated no relevant financial relationships.
Barath Prashanth Sivasubramanian indicated no relevant financial relationships.
Jaskaranpreet Kaur, MD, MS1, Navneet Kaur, MD1, Sheena Bhushan, MD2, Barath Prashanth Sivasubramanian, MD2. P2258 - Rapidly Growing Adenocarcinoma at the Gastroesophageal Junction 18 Years After Roux-en-Y Gastric Bypass: A Case Report and Review of Surveillance Necessities, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
