Monday Poster Session
Category: Esophagus
P2265 - Killian-Jamieson Diverticulum and Cricopharyngeal Dysfunction: A Case Report of Clinical Conundrum
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PZ
Pan Zonghao, MD
Temple University/Conemaugh Memorial Medical Center Internal Medicine
Johnstown, PA
Presenting Author(s)
Pan Zonghao, MD1, Chuong Le, MD1, Muhammad Zaman, MD1, Warsha Korani, MD1, Tarek Alansari, MD2
1Temple University/Conemaugh Memorial Medical Center Internal Medicine, Johnstown, PA; 2Conemaugh Memorial Medical Center, Johnstown, PA
Introduction: There is a theoretical yet unconfirmed link between Killian-Jamieson diverticulum (KJD) and cricopharyngeal dysfunction, both of which can cause oropharyngeal dysphagia or remain asymptomatic, posing a diagnostic challenge. It's crucial to accurately identify the source of dysphagia and assess for reversible causes before considering surgery for KJD.
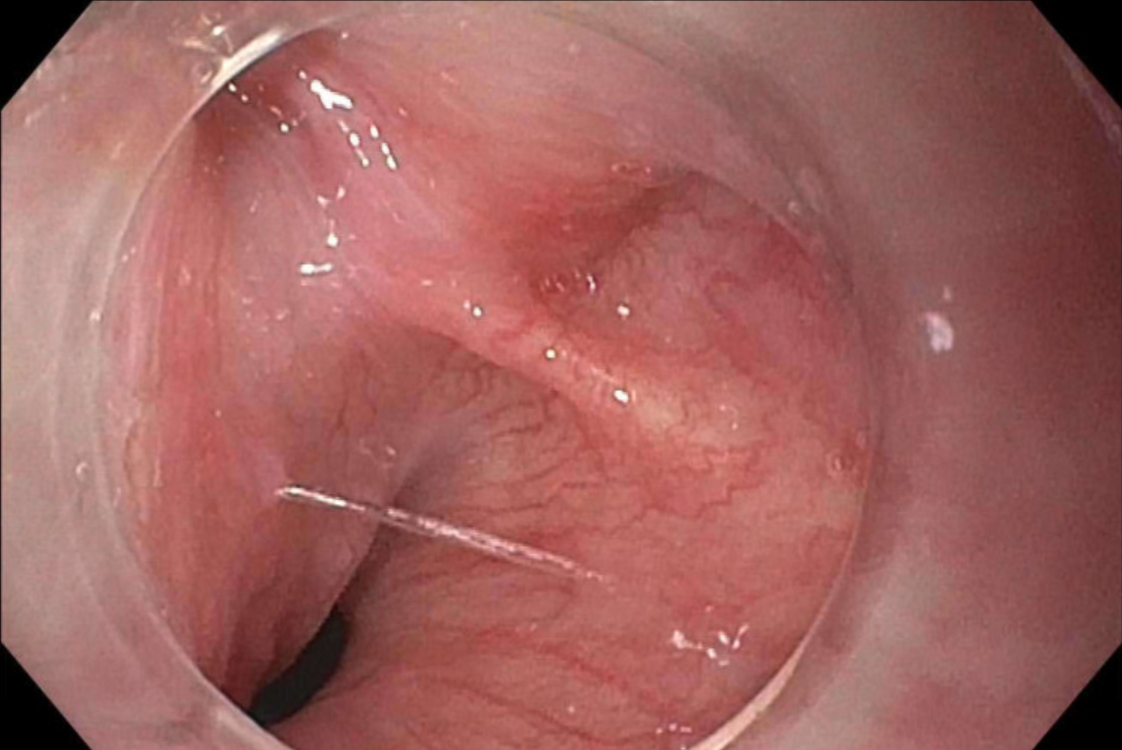
Case Description/Methods: A 79-year-old woman with a family history of gastric cancer was hospitalized after a fall, reporting worsening dysphagia to solid food and a 15-pound weight loss over one month. She was on pantoprazole 40 mg daily for GERD. At admission, she had acute kidney injury, sepsis from aspiration pneumonia, and fluid-responsive hypotension. A barium swallow test showed minimal pharyngeal residue and silent aspiration. The patient was able to clear all aspirated material when prompted to clear her throat. EGD revealed a hypertonic upper esophageal sphincter, a 1.5 cm KJD at the cricopharyngeus, and patchy severe inflammation with adherent blood and erosions in the gastric antrum. Given her age and other medical conditions, she opted for conservative management with pantoprazole 40mg twice daily. A month later, her dysphagia had resolved, and she regained 20 pounds.
Discussion: First described in 1983, KJD is a rare esophageal diverticulum arising from the lateral Killian-Jamieson space near the cricoid cartilage and inferior laryngeal nerve. KJD's occurrence is about 2% in patients with pharyngeal dysphagia, and its development might be linked to cricopharyngeal dysfunction. This connection has led some to suggest cricopharyngeal myotomy with diverticulectomy to potentially prevent complications like Zenker’s diverticulum (ZD), although debatable. Most individuals with KJD (89%) exhibit no symptoms and typically do not need intervention. Unlike ZD, aspiration pneumonia is uncommon in KJD, likely due to its small size and specific location. For symptomatic cases, treatment options include endoscopic or surgical diverticulectomy.
In our case, a patient with dysphagia, weight loss, and pneumonia was found to have KJD and a hypertonic upper esophageal sphincter. Despite these findings, symptoms improved with increased pantoprazole, indicating that the issue was more likely due to cricopharyngeal dysfunction from uncontrolled GERD rather than KJD. While surgery is definitive for symptomatic KJD, assessing other potential causes of dysphagia is crucial before considering surgical intervention.
Disclosures:
Pan Zonghao, MD1, Chuong Le, MD1, Muhammad Zaman, MD1, Warsha Korani, MD1, Tarek Alansari, MD2. P2265 - Killian-Jamieson Diverticulum and Cricopharyngeal Dysfunction: A Case Report of Clinical Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Temple University/Conemaugh Memorial Medical Center Internal Medicine, Johnstown, PA; 2Conemaugh Memorial Medical Center, Johnstown, PA
Introduction: There is a theoretical yet unconfirmed link between Killian-Jamieson diverticulum (KJD) and cricopharyngeal dysfunction, both of which can cause oropharyngeal dysphagia or remain asymptomatic, posing a diagnostic challenge. It's crucial to accurately identify the source of dysphagia and assess for reversible causes before considering surgery for KJD.
Case Description/Methods: A 79-year-old woman with a family history of gastric cancer was hospitalized after a fall, reporting worsening dysphagia to solid food and a 15-pound weight loss over one month. She was on pantoprazole 40 mg daily for GERD. At admission, she had acute kidney injury, sepsis from aspiration pneumonia, and fluid-responsive hypotension. A barium swallow test showed minimal pharyngeal residue and silent aspiration. The patient was able to clear all aspirated material when prompted to clear her throat. EGD revealed a hypertonic upper esophageal sphincter, a 1.5 cm KJD at the cricopharyngeus, and patchy severe inflammation with adherent blood and erosions in the gastric antrum. Given her age and other medical conditions, she opted for conservative management with pantoprazole 40mg twice daily. A month later, her dysphagia had resolved, and she regained 20 pounds.
Discussion: First described in 1983, KJD is a rare esophageal diverticulum arising from the lateral Killian-Jamieson space near the cricoid cartilage and inferior laryngeal nerve. KJD's occurrence is about 2% in patients with pharyngeal dysphagia, and its development might be linked to cricopharyngeal dysfunction. This connection has led some to suggest cricopharyngeal myotomy with diverticulectomy to potentially prevent complications like Zenker’s diverticulum (ZD), although debatable. Most individuals with KJD (89%) exhibit no symptoms and typically do not need intervention. Unlike ZD, aspiration pneumonia is uncommon in KJD, likely due to its small size and specific location. For symptomatic cases, treatment options include endoscopic or surgical diverticulectomy.
In our case, a patient with dysphagia, weight loss, and pneumonia was found to have KJD and a hypertonic upper esophageal sphincter. Despite these findings, symptoms improved with increased pantoprazole, indicating that the issue was more likely due to cricopharyngeal dysfunction from uncontrolled GERD rather than KJD. While surgery is definitive for symptomatic KJD, assessing other potential causes of dysphagia is crucial before considering surgical intervention.
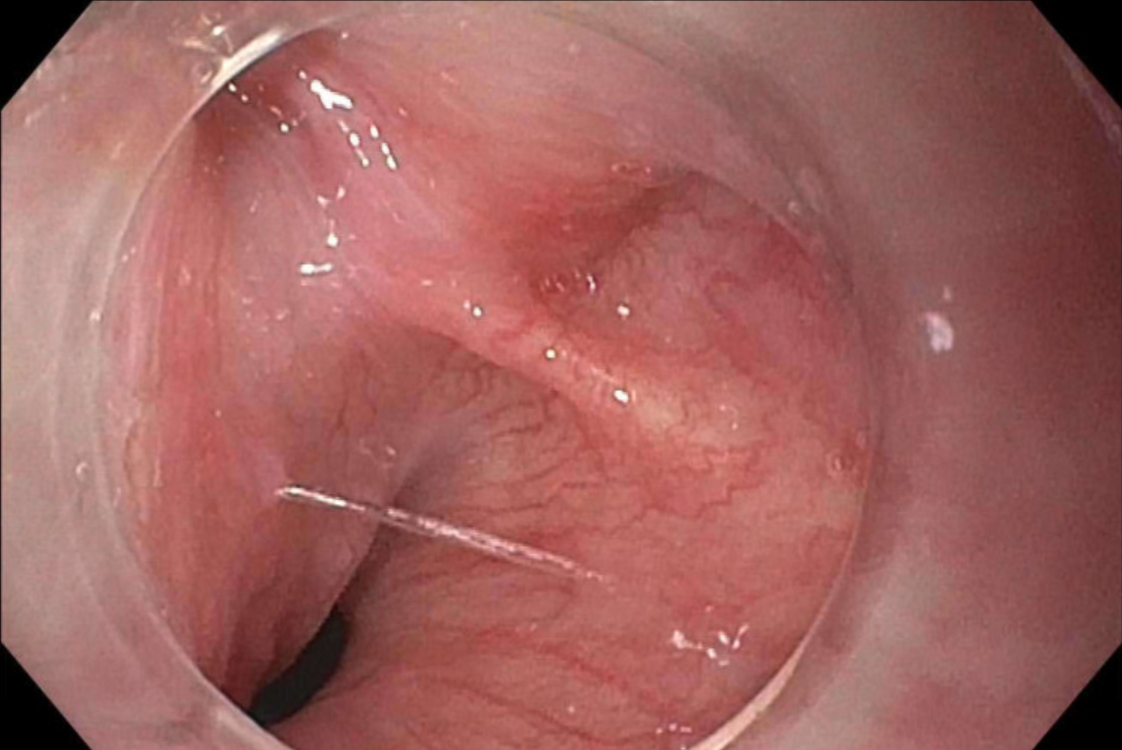
Figure: Fig 1. EGD revealed a 1.5 cm Killian-Jamieson diverticulum at the cricopharyngeus
Disclosures:
Pan Zonghao indicated no relevant financial relationships.
Chuong Le indicated no relevant financial relationships.
Muhammad Zaman indicated no relevant financial relationships.
Warsha Korani indicated no relevant financial relationships.
Tarek Alansari indicated no relevant financial relationships.
Pan Zonghao, MD1, Chuong Le, MD1, Muhammad Zaman, MD1, Warsha Korani, MD1, Tarek Alansari, MD2. P2265 - Killian-Jamieson Diverticulum and Cricopharyngeal Dysfunction: A Case Report of Clinical Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
