Monday Poster Session
Category: Esophagus
P2268 - A Misleading Path: Blown Out Myotomy (BOM) Disguised as a Slipped Nissen
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DS
Daniel Staursky, DO
Medical College of Georgia
Augusta, GA
Presenting Author(s)
Daniel Staursky, DO1, Dhanush Shimoga, MBBS2, Amol Sharma, MS, MD, FACG2
1Medical College of Georgia, Augusta, GA; 2Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Heller myotomy and Nissen fundoplication (NF) are common surgical treatments for achalasia and gastroesophageal reflux disease (GERD). Post-surgical complications include a migration or herniation of the Nissen wrap or blown out myotomy (BOM). We present a delayed presentation of recurrent achalasia symptoms secondary to a BOM.
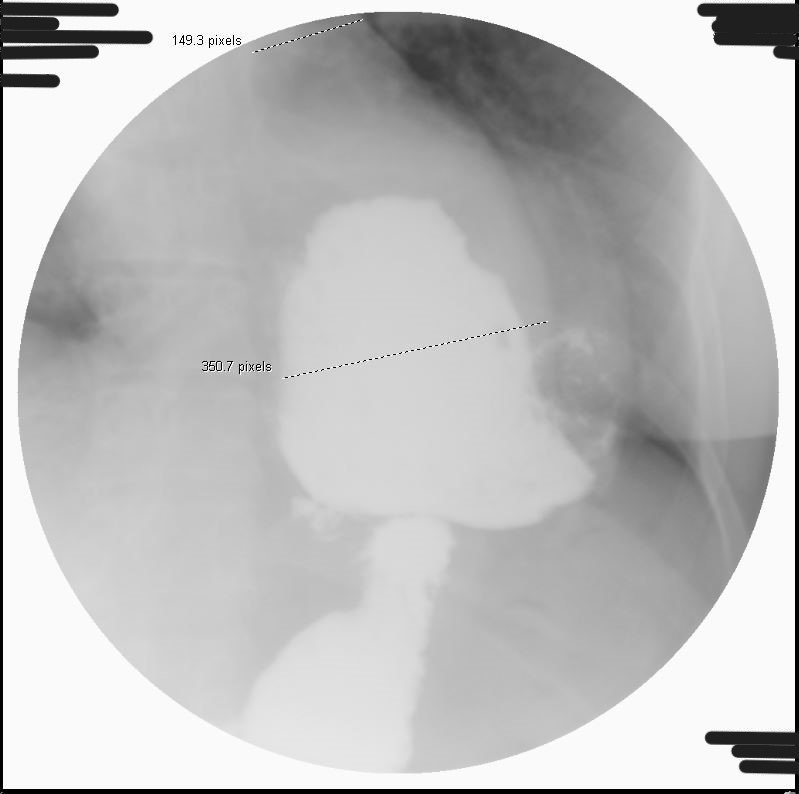
Case Description/Methods: A 43-year old female with history of achalasia status post Heller myotomy and Nissen fundoplication 25 years prior presented with increasing dysphagia to solids and liquids, chest discomfort and daily regurgitation. Physical exam was unremarkable. High-resolution esophageal manometry (HREM) was obtained. Normal IRP of the EGJ was noted. HREM also demonstrated 100% absent peristalsis and 0% bolus clearance. Interpretation of the study was abnormal, consistent with absent contractility and low resting lower esophageal sphincter pressure. EGD was aborted due to a large amount of food in the distal esophagus despite a clear liquid diet (CLD) 2 days prior to procedure. A barium esophagram showed large infra-diaphragmatic, contrast-filled gastric pouch with mid gastric body luminal anatomy narrowing, suggestive of slipped Nissen "Hinder Type III", delayed esophageal transit and large volume spontaneous GERD favored secondary to wrap slippage, shown in Figure 1. Repeat EGD with extended clear liquid diet prior noted a tortuous, sigmoid, dilated esophagus with mild esophagitis. Endoscope was able to traverse the EGJ at 45cm from incisors without resistance. Normal antrum, body, fundus and cardia on retroflex view and normal duodenum noted.
Discussion: BOM is an under-recognized complication of laparascopic Heller myotomy and 15-20% of peroral endoscopic myotomy (POEM) procedures with the formation of a pseudodiverticulum at the myotomy site1. Radiology plays a critical role in diagnosis and BOM is defined as a >50% increase in esophageal diameter on esophagram. This case highlights the need for increased awareness of this condition as POEM becomes more adopted into clinical management of achalasia.
1. Krause, Amanda J., et al. "423 Blown out Myotomy (BOM), a Complication Following Laparoscopic Heller Myotomy and Per-Oral Endoscopic Myotomy." Official journal of the American College of Gastroenterology| ACG 114 (2019): S248-S249.
Disclosures:
Daniel Staursky, DO1, Dhanush Shimoga, MBBS2, Amol Sharma, MS, MD, FACG2. P2268 - A Misleading Path: Blown Out Myotomy (BOM) Disguised as a Slipped Nissen, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Georgia, Augusta, GA; 2Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Heller myotomy and Nissen fundoplication (NF) are common surgical treatments for achalasia and gastroesophageal reflux disease (GERD). Post-surgical complications include a migration or herniation of the Nissen wrap or blown out myotomy (BOM). We present a delayed presentation of recurrent achalasia symptoms secondary to a BOM.
Case Description/Methods: A 43-year old female with history of achalasia status post Heller myotomy and Nissen fundoplication 25 years prior presented with increasing dysphagia to solids and liquids, chest discomfort and daily regurgitation. Physical exam was unremarkable. High-resolution esophageal manometry (HREM) was obtained. Normal IRP of the EGJ was noted. HREM also demonstrated 100% absent peristalsis and 0% bolus clearance. Interpretation of the study was abnormal, consistent with absent contractility and low resting lower esophageal sphincter pressure. EGD was aborted due to a large amount of food in the distal esophagus despite a clear liquid diet (CLD) 2 days prior to procedure. A barium esophagram showed large infra-diaphragmatic, contrast-filled gastric pouch with mid gastric body luminal anatomy narrowing, suggestive of slipped Nissen "Hinder Type III", delayed esophageal transit and large volume spontaneous GERD favored secondary to wrap slippage, shown in Figure 1. Repeat EGD with extended clear liquid diet prior noted a tortuous, sigmoid, dilated esophagus with mild esophagitis. Endoscope was able to traverse the EGJ at 45cm from incisors without resistance. Normal antrum, body, fundus and cardia on retroflex view and normal duodenum noted.
Discussion: BOM is an under-recognized complication of laparascopic Heller myotomy and 15-20% of peroral endoscopic myotomy (POEM) procedures with the formation of a pseudodiverticulum at the myotomy site1. Radiology plays a critical role in diagnosis and BOM is defined as a >50% increase in esophageal diameter on esophagram. This case highlights the need for increased awareness of this condition as POEM becomes more adopted into clinical management of achalasia.
1. Krause, Amanda J., et al. "423 Blown out Myotomy (BOM), a Complication Following Laparoscopic Heller Myotomy and Per-Oral Endoscopic Myotomy." Official journal of the American College of Gastroenterology| ACG 114 (2019): S248-S249.
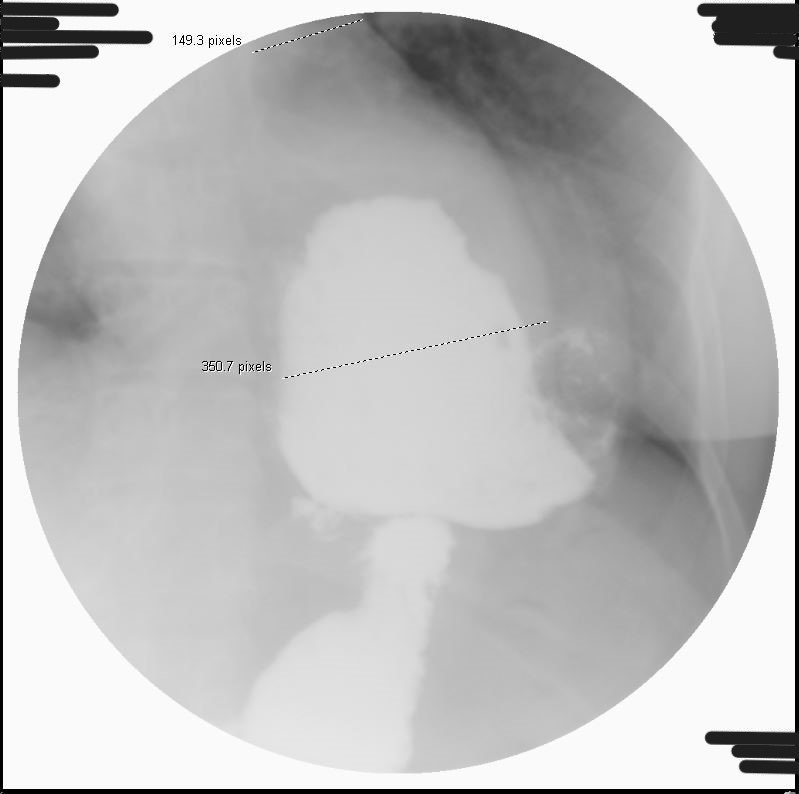
Figure: Figure 1: BOM on esophagram with >50% increase in esophageal diameter in distal esophagus compared to mid-esophagus
Disclosures:
Daniel Staursky indicated no relevant financial relationships.
Dhanush Shimoga indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Daniel Staursky, DO1, Dhanush Shimoga, MBBS2, Amol Sharma, MS, MD, FACG2. P2268 - A Misleading Path: Blown Out Myotomy (BOM) Disguised as a Slipped Nissen, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
