Monday Poster Session
Category: Esophagus
P2286 - Para-Esophageal Abscess Causing Dysphagia From Post-Operative Complication of CABG Surgery
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gurjot Singh, DO
The Warren Alpert Medical School of Brown University
Warwick, RI
Presenting Author(s)
Gurjot Singh, DO1, Tamara Koritarov, DO2, Muhammad Zain Ali, MBChB1
1The Warren Alpert Medical School of Brown University, Warwick, RI; 2Kent Hospital, Warwick, RI
Introduction: Coronary artery bypass graft (CABG) surgery is a procedure performed for revascularization in multivessel disease with the most common reason for readmission being postoperative infection. This case explores a patient who underwent a CABG and developed a rare complication leading to dysphagia secondary to abscess formation.
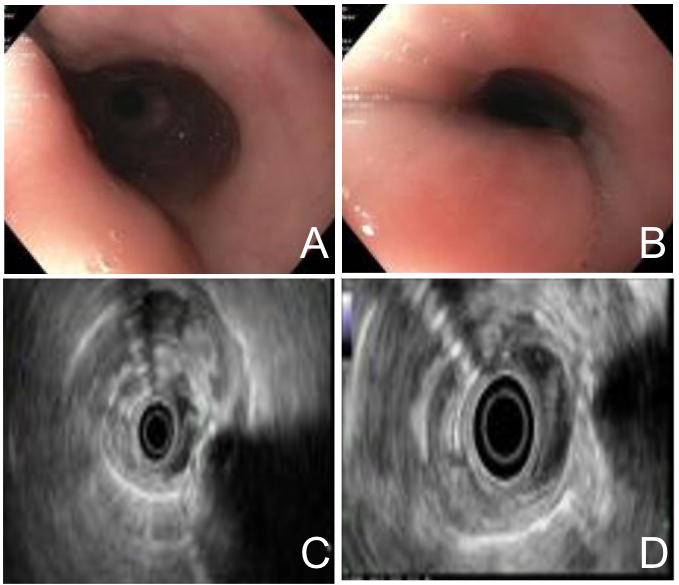
Case Description/Methods: A 75-year-old male, 1 month post-op from CABG surgery presented with complaints of chills, nausea, and vomiting. Past medical history included congestive heart failure with reduced ejection fraction, coronary artery disease, type 2 diabetes, hypertension, hyperlipidemia, and prior DVT. Vitals on admission were stable. Laboratory studies revealed a leukocytosis of 23.3x10^3/mcL with an absolute neutrophil count of 20.0x10^3/mcL, and hemoglobin at baseline. On admission, broad spectrum antibiotics were started with Vancomycin and Zosyn and blood cultures collected. Six hours postadmission, the patient developed new onset dysphagia. A full neurological examination was unremarkable. Dysphagia was greater with solids than liquids with no odynophagia. Modified barium swallow (MBS) demonstrated laryngeal penetration and aspiration with large bolus of thin liquids. Blood cultures demonstrated growth of methicillin-susceptible Staphylococcus aureus (MSSA). EGD revealed an extrinsic compression of the second and third portion of the esophagus. Endoscopic ultrasound demonstrated an intramural subepithelial lesion that was anechoic in nature with well-defined borders, most consistent with a fluid-filled lesion. Patient was discharged with a PICC line and antibiotics infusions to be completed outpatient with a repeat CT scan 2 weeks later. Repeat CT demonstrated increased densities with internal air locules with increasing size of fluid-collection measuring 5.0 x 3.0 x 3.3 cm. Cardiothoracic surgery was consulted and para-esophageal fluid was drained with cultures growing MSSA. Patient received cefazolin for 4 weeks from source control.
Discussion: Esophageal dysphagia can be broadly classified into 2 categories: motility or mechanical/structural causes. Motility causes are often secondary to neuromuscular deficits, such as in achalasia with dysphagia mainly to both solids and liquids. In mechanical/structural causes patients have difficulty ingesting solids greater than liquids, similar to the patient in this case. Structural causes include intrinsic or extrinsic, such as malignancy, or an unsuspecting diagnosis of a para-esophageal abscess post-CABG surgery.
Disclosures:
Gurjot Singh, DO1, Tamara Koritarov, DO2, Muhammad Zain Ali, MBChB1. P2286 - Para-Esophageal Abscess Causing Dysphagia From Post-Operative Complication of CABG Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Warren Alpert Medical School of Brown University, Warwick, RI; 2Kent Hospital, Warwick, RI
Introduction: Coronary artery bypass graft (CABG) surgery is a procedure performed for revascularization in multivessel disease with the most common reason for readmission being postoperative infection. This case explores a patient who underwent a CABG and developed a rare complication leading to dysphagia secondary to abscess formation.
Case Description/Methods: A 75-year-old male, 1 month post-op from CABG surgery presented with complaints of chills, nausea, and vomiting. Past medical history included congestive heart failure with reduced ejection fraction, coronary artery disease, type 2 diabetes, hypertension, hyperlipidemia, and prior DVT. Vitals on admission were stable. Laboratory studies revealed a leukocytosis of 23.3x10^3/mcL with an absolute neutrophil count of 20.0x10^3/mcL, and hemoglobin at baseline. On admission, broad spectrum antibiotics were started with Vancomycin and Zosyn and blood cultures collected. Six hours postadmission, the patient developed new onset dysphagia. A full neurological examination was unremarkable. Dysphagia was greater with solids than liquids with no odynophagia. Modified barium swallow (MBS) demonstrated laryngeal penetration and aspiration with large bolus of thin liquids. Blood cultures demonstrated growth of methicillin-susceptible Staphylococcus aureus (MSSA). EGD revealed an extrinsic compression of the second and third portion of the esophagus. Endoscopic ultrasound demonstrated an intramural subepithelial lesion that was anechoic in nature with well-defined borders, most consistent with a fluid-filled lesion. Patient was discharged with a PICC line and antibiotics infusions to be completed outpatient with a repeat CT scan 2 weeks later. Repeat CT demonstrated increased densities with internal air locules with increasing size of fluid-collection measuring 5.0 x 3.0 x 3.3 cm. Cardiothoracic surgery was consulted and para-esophageal fluid was drained with cultures growing MSSA. Patient received cefazolin for 4 weeks from source control.
Discussion: Esophageal dysphagia can be broadly classified into 2 categories: motility or mechanical/structural causes. Motility causes are often secondary to neuromuscular deficits, such as in achalasia with dysphagia mainly to both solids and liquids. In mechanical/structural causes patients have difficulty ingesting solids greater than liquids, similar to the patient in this case. Structural causes include intrinsic or extrinsic, such as malignancy, or an unsuspecting diagnosis of a para-esophageal abscess post-CABG surgery.
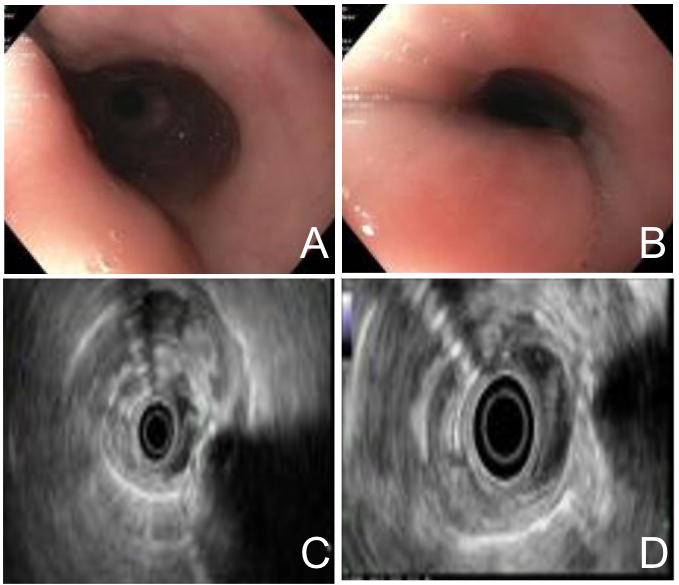
Figure: A.) and B.) Multi views of extrinsic compression observed at second and third portion of esophagus via EGD.
C.) and D.) Multi views of endoscopic ultrasound demonstrating a well-defined fluid-filled lesion.
C.) and D.) Multi views of endoscopic ultrasound demonstrating a well-defined fluid-filled lesion.
Disclosures:
Gurjot Singh indicated no relevant financial relationships.
Tamara Koritarov indicated no relevant financial relationships.
Muhammad Zain Ali indicated no relevant financial relationships.
Gurjot Singh, DO1, Tamara Koritarov, DO2, Muhammad Zain Ali, MBChB1. P2286 - Para-Esophageal Abscess Causing Dysphagia From Post-Operative Complication of CABG Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
