Monday Poster Session
Category: Esophagus
P2292 - Black Esophagus - A Rare Cause of Upper GI Bleeding in the Metastatic Pancreatic Cancer after Initiation of FOLFIRINOX Chemotherapy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RF
Rida Fatima, MD
Bassett Medical Center
Cooperstown, NY
Presenting Author(s)
Rida Fatima, MD1, Muhammad Bilal, MD1, Azhar Hussain, MBBS2, Saurav Kini, MD3, Peter Francisco, DO1
1Bassett Medical Center, Cooperstown, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3Tufts Medical Center, Boston, MA
Introduction: Black esophagus, a rare clinical condition with an unclear incidence or prevalence, is characterized by the diffuse circumferential black appearance of the esophageal mucosa. It typically presents as upper gastrointestinal bleeding. Risk factors include hypertension, coronary artery disease, diabetes mellitus, and underlying malignancy. Complications include the formation of esophageal strictures and esophageal perforation. We present a case of black esophagus after initiation of FOLFIRINOX in pancreatic cancer, a potential association that has not been widely reported.
Case Description/Methods: 81-year-old female with a past medical history significant for hypertension, type 2 diabetes mellitus, and recently diagnosed metastatic pancreatic cancer on chemotherapy presented to the hospital with hematemesis and melena. On presentation, the patient was vitally stable. Physical examination was unremarkable.
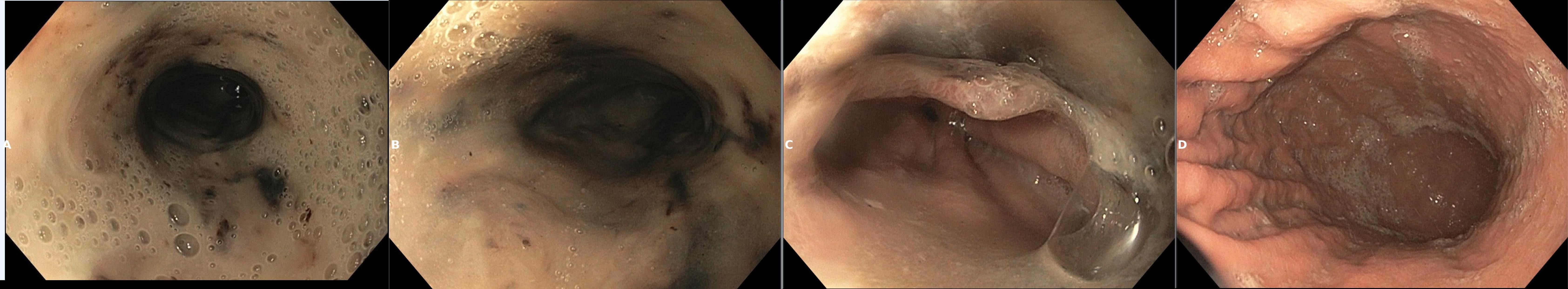
On presentation, the patient's hemoglobin was 8.0 g/dl, with baseline hemoglobin was around 10 g/dl. CT Abdomen with IV contrast showed an interval increase in pancreatic head mass size. The patient was started on IV pantoprazole 40 mg twice daily and an octreotide infusion. Esophagogastroduodenoscopy (EGD) was done the next day, which showed a black esophagus appreciated from the proximal esophagus down to the gastroesophageal junction without any active bleeding; the stomach and duodenum appeared normal. EGD done at the time of pancreatic cancer diagnosis was unremarkable. The patient tolerated oral intake with stable hemodynamic status and hemoglobin over the hospital course. The patient was discharged on pantoprazole and sucralfate suspension with follow-up EGD in 1-2 months. Unfortunately, the patient died before her repeat EGD.
Discussion: Post-Chemotherapy black esophagus, including FOLFIRINOX, has been reported in only a few case reports and series1. Although no proper data on black esophagus mortality is available, it usually indicates a poor prognosis. Treatment is generally conservative with fluid resuscitation/blood transfusion if needed, avoiding hypotension, early initiation of proton pump inhibitors, and timely EGD. Follow-up EGD is usually done in 1-2 months. In transmural necrosis of the esophagus, diligent EGD should be done due to the risk of esophageal perforation and the patient should be carefully monitored.
1- Forys OC, Ferguson DD. Black Esophagus Associated with Malignancy and Use of FOLFOX/Avastin. Am J Gastroenterol. 2007 Sep;102(Suppl):S125.
Disclosures:
Rida Fatima, MD1, Muhammad Bilal, MD1, Azhar Hussain, MBBS2, Saurav Kini, MD3, Peter Francisco, DO1. P2292 - Black Esophagus - A Rare Cause of Upper GI Bleeding in the Metastatic Pancreatic Cancer after Initiation of FOLFIRINOX Chemotherapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Bassett Medical Center, Cooperstown, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3Tufts Medical Center, Boston, MA
Introduction: Black esophagus, a rare clinical condition with an unclear incidence or prevalence, is characterized by the diffuse circumferential black appearance of the esophageal mucosa. It typically presents as upper gastrointestinal bleeding. Risk factors include hypertension, coronary artery disease, diabetes mellitus, and underlying malignancy. Complications include the formation of esophageal strictures and esophageal perforation. We present a case of black esophagus after initiation of FOLFIRINOX in pancreatic cancer, a potential association that has not been widely reported.
Case Description/Methods: 81-year-old female with a past medical history significant for hypertension, type 2 diabetes mellitus, and recently diagnosed metastatic pancreatic cancer on chemotherapy presented to the hospital with hematemesis and melena. On presentation, the patient was vitally stable. Physical examination was unremarkable.
On presentation, the patient's hemoglobin was 8.0 g/dl, with baseline hemoglobin was around 10 g/dl. CT Abdomen with IV contrast showed an interval increase in pancreatic head mass size. The patient was started on IV pantoprazole 40 mg twice daily and an octreotide infusion. Esophagogastroduodenoscopy (EGD) was done the next day, which showed a black esophagus appreciated from the proximal esophagus down to the gastroesophageal junction without any active bleeding; the stomach and duodenum appeared normal. EGD done at the time of pancreatic cancer diagnosis was unremarkable. The patient tolerated oral intake with stable hemodynamic status and hemoglobin over the hospital course. The patient was discharged on pantoprazole and sucralfate suspension with follow-up EGD in 1-2 months. Unfortunately, the patient died before her repeat EGD.
Discussion: Post-Chemotherapy black esophagus, including FOLFIRINOX, has been reported in only a few case reports and series1. Although no proper data on black esophagus mortality is available, it usually indicates a poor prognosis. Treatment is generally conservative with fluid resuscitation/blood transfusion if needed, avoiding hypotension, early initiation of proton pump inhibitors, and timely EGD. Follow-up EGD is usually done in 1-2 months. In transmural necrosis of the esophagus, diligent EGD should be done due to the risk of esophageal perforation and the patient should be carefully monitored.
1- Forys OC, Ferguson DD. Black Esophagus Associated with Malignancy and Use of FOLFOX/Avastin. Am J Gastroenterol. 2007 Sep;102(Suppl):S125.
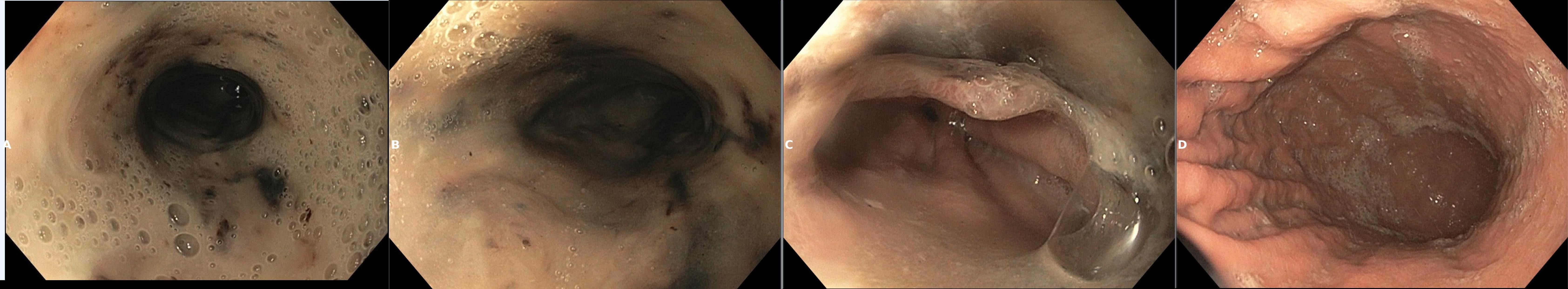
Figure: Figure 1. A, B, C showing Upper, middle third of esophagus and gastroesophageal junction showing black esophagus. D) normal gastric body
Disclosures:
Rida Fatima indicated no relevant financial relationships.
Muhammad Bilal indicated no relevant financial relationships.
Azhar Hussain indicated no relevant financial relationships.
Saurav Kini indicated no relevant financial relationships.
Peter Francisco indicated no relevant financial relationships.
Rida Fatima, MD1, Muhammad Bilal, MD1, Azhar Hussain, MBBS2, Saurav Kini, MD3, Peter Francisco, DO1. P2292 - Black Esophagus - A Rare Cause of Upper GI Bleeding in the Metastatic Pancreatic Cancer after Initiation of FOLFIRINOX Chemotherapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
