Monday Poster Session
Category: Esophagus
P2295 - Behçet’s Disease: A Rare Case of Esophageal Involvement
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Charles B. Woodall, DO
Louisiana State University Health Sciences Center
Covington, LA
Presenting Author(s)
Charles B. Woodall, DO1, Nikki Arceneaux, MD2, Hunter Hall, MD3, Jason Stibbe, MD4
1Louisiana State University Health Sciences Center, Covington, LA; 2Louisiana State University Health Sciences Center, New Orleans, LA; 3LSU, New Orleans, LA; 4LSU Health New Orleans School of Medicine, New Orleans, LA
Introduction: Behçet’s disease (BD) is a chronic inflammatory condition driven by systemic vasculitis that affects vessels of all size. Typical manifestations include orogenital ulcers, uveitis, and cutaneous lesions, but GI manifestations can also be seen. Esophageal Behçet’s disease (EBD) is rare and typically causes symptoms of pain and dysphagia due to ulceration of the esophageal mucosa, but more serious complications such as perforation and stricture can also occur.
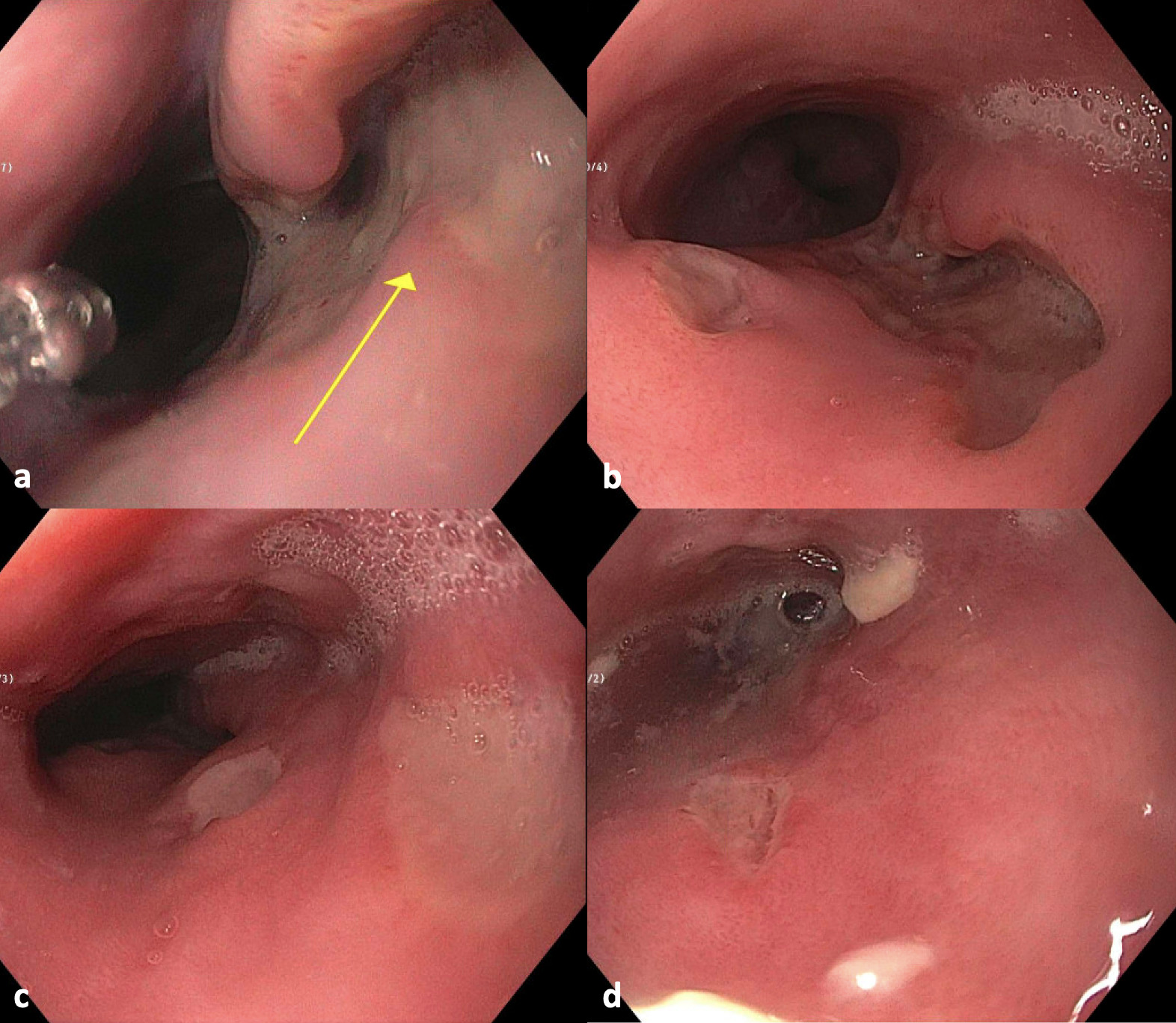
Case Description/Methods: A 41-year-old female with a history of BD with previous orogenital and ileal manifestations presented with epigastric pain and odynophagia for one week as well as pustules on her chest, forehead, and right eyelid. She previously followed with rheumatology at which time she underwent a short duration of apremilast therapy but had been lost to follow up for two years. She was started on prednisone at admission and thiopurine methyltransferase (TPMT) activity was assessed in anticipation of starting azathioprine. EGD demonstrated superficial, cratered ulcers in the esophagus with the largest measuring 15 mm. Sucralfate and pantoprazole were started, and she was discharged with rheumatology follow up where she was continued on prednisone and started on azathioprine. Close monitoring of her blood count was planned given mildly decreased TPMT activity, but she was lost to follow up again thereafter.
Discussion: Ileocecal involvement is the most common GI manifestation in BD. Esophageal lesions are rare, and gastric involvement is the least common. The incidence of EBD is low, but usually involves the middle portion of the esophagus. Common symptoms include dysphagia and substernal chest pain, but hematemesis due to ulceration is also seen. Complications such as perforation, fistulization, and stricture are also described in the literature but are rare. Endoscopy is necessary to assess the extent and severity of damage. Proton pump inhibitors and aminosalicylates are used as first-line agents in mild to moderate EBD. Management of moderate to severe EBD relies on glucocorticoids for immediate immune suppression and reduction of inflammation along with long-term azathioprine to limit glucocorticoid use. TNF-alpha inhibitors and nutrition therapy are also used but are reserved for cases refractory to first-line agents. Surgery is indicated in cases that fail medical management and those with serious complications. Postoperative rates of recurrence are high, and continued medical therapy is necessary to mitigate the risk.
Disclosures:
Charles B. Woodall, DO1, Nikki Arceneaux, MD2, Hunter Hall, MD3, Jason Stibbe, MD4. P2295 - Behçet’s Disease: A Rare Case of Esophageal Involvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Louisiana State University Health Sciences Center, Covington, LA; 2Louisiana State University Health Sciences Center, New Orleans, LA; 3LSU, New Orleans, LA; 4LSU Health New Orleans School of Medicine, New Orleans, LA
Introduction: Behçet’s disease (BD) is a chronic inflammatory condition driven by systemic vasculitis that affects vessels of all size. Typical manifestations include orogenital ulcers, uveitis, and cutaneous lesions, but GI manifestations can also be seen. Esophageal Behçet’s disease (EBD) is rare and typically causes symptoms of pain and dysphagia due to ulceration of the esophageal mucosa, but more serious complications such as perforation and stricture can also occur.
Case Description/Methods: A 41-year-old female with a history of BD with previous orogenital and ileal manifestations presented with epigastric pain and odynophagia for one week as well as pustules on her chest, forehead, and right eyelid. She previously followed with rheumatology at which time she underwent a short duration of apremilast therapy but had been lost to follow up for two years. She was started on prednisone at admission and thiopurine methyltransferase (TPMT) activity was assessed in anticipation of starting azathioprine. EGD demonstrated superficial, cratered ulcers in the esophagus with the largest measuring 15 mm. Sucralfate and pantoprazole were started, and she was discharged with rheumatology follow up where she was continued on prednisone and started on azathioprine. Close monitoring of her blood count was planned given mildly decreased TPMT activity, but she was lost to follow up again thereafter.
Discussion: Ileocecal involvement is the most common GI manifestation in BD. Esophageal lesions are rare, and gastric involvement is the least common. The incidence of EBD is low, but usually involves the middle portion of the esophagus. Common symptoms include dysphagia and substernal chest pain, but hematemesis due to ulceration is also seen. Complications such as perforation, fistulization, and stricture are also described in the literature but are rare. Endoscopy is necessary to assess the extent and severity of damage. Proton pump inhibitors and aminosalicylates are used as first-line agents in mild to moderate EBD. Management of moderate to severe EBD relies on glucocorticoids for immediate immune suppression and reduction of inflammation along with long-term azathioprine to limit glucocorticoid use. TNF-alpha inhibitors and nutrition therapy are also used but are reserved for cases refractory to first-line agents. Surgery is indicated in cases that fail medical management and those with serious complications. Postoperative rates of recurrence are high, and continued medical therapy is necessary to mitigate the risk.
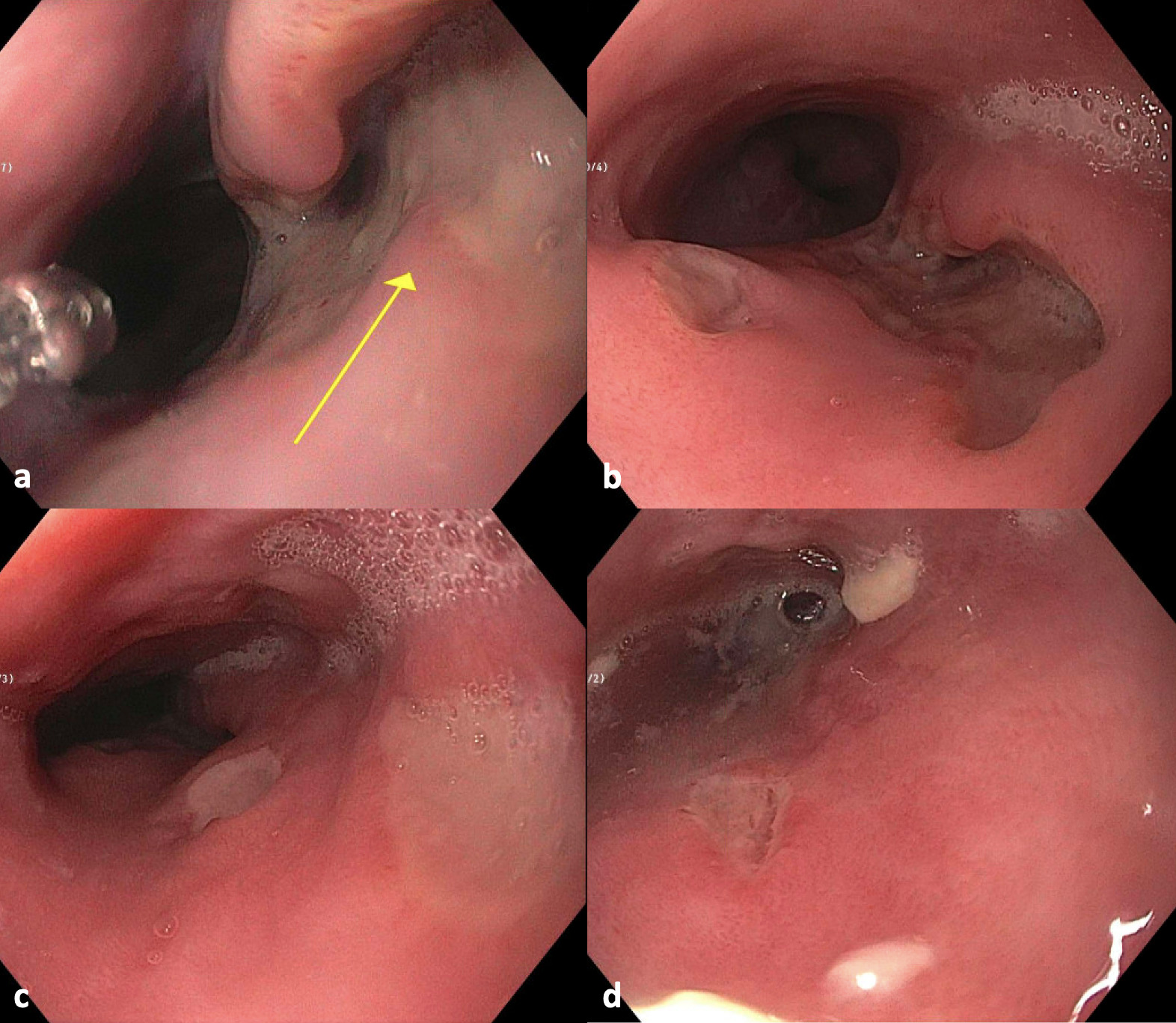
Figure: a. Largest ulceration (15 mm) in the lower third of esophagus just proximal to GE junction; b. Alternate view of largest ulceration; c. Additional ulcerations in lower third of esophagus; d. Ulceration in middle third of the esophagus
Disclosures:
Charles Woodall indicated no relevant financial relationships.
Nikki Arceneaux indicated no relevant financial relationships.
Hunter Hall indicated no relevant financial relationships.
Jason Stibbe indicated no relevant financial relationships.
Charles B. Woodall, DO1, Nikki Arceneaux, MD2, Hunter Hall, MD3, Jason Stibbe, MD4. P2295 - Behçet’s Disease: A Rare Case of Esophageal Involvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
