Monday Poster Session
Category: Esophagus
P2299 - Is It a Wrap? Achalasia Management After Sleeve Gastrectomy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Stavros Doumas, MD, MS, PhD
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Stavros Doumas, MD, MS, PhD1, Corinne O'Connor, MD1, Fredrick Brody, MD2, Marianna Papademetriou, MD2
1MedStar Georgetown University Hospital, Washington, DC; 2Washington DC VA Medical Center, Washington, DC
Introduction: Esophageal dysmotility is an established complication following gastric bypass and banding and recently reported after laparoscopic sleeve gastrectomy (LSG). Dysphagia and associated dysmotility can range from mild to severe. Severe cases may reflect the evolution of primary achalasia or elevated intragastric pressure with aperistalsis, recently termed post-obesity esophageal dysfunction (POSED). Achalasia following-LSG constitutes a surgical challenge as the absence of the fundus prohibits the addition of a fundoplication in conjunction with a Heller myotomy. We report the case of a young female who developed achalasia following LSG.
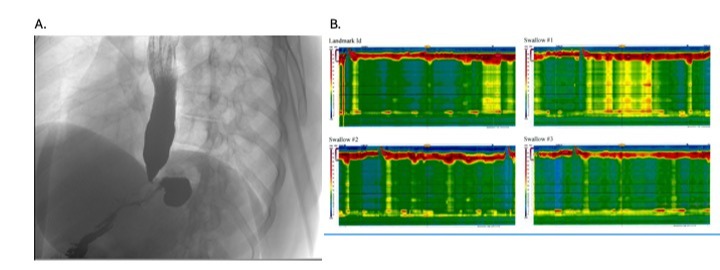
Case Description/Methods: A 34-year-old woman with a long-standing GERD and obesity for which she underwent LSG four years prior presented with a two-month history of progressively worsening dysphagia to solids and liquids and precipitous weight loss. The patient denied dysphagia prior to surgery. She received Omeprazole empirically, without relief, and underwent an EGD, which demonstrated grade D esophagitis. Biopsies were positive for Candida, and she was started on pantoprazole and fluconazole. At two weeks follow-up, she reported persistent symptoms and underwent a repeat EGD with empiric balloon dilation of the LES (12mm to 15mm) without symptom improvement. She underwent an esophageal manometry that showed an IRP of 19.4mmHg with 100% failed esophageal motility with pan esophageal pressurization without elevated intragastric pressure, consistent with Type 2 Achalasia. The patient underwent a laparoscopic Heller Myotomy with plication of the myotomy site to the diaphragmatic crura with sutures to mimic the tension created by a fundoplication. The patient’s post-operative course was uncomplicated, and she reported significant improvement of her dysphagia.
Discussion: Severe esophageal dysmotility is increasingly recognized in patients undergoing LSG. Achalasia remains rare after bariatric surgery; however, it appears that surgery may be a risk factor. Because our patient had an elevated IRP and normal intragastric pressure, we elected to treat this patient as primary achalasia. It is currently unclear which patients are at risk of developing esophageal dysmotility. Management of achalasia in the setting of prior LSG poses a particular surgical challenge. Future studies are needed to identify the patients at risk of developing post-LSG esophageal dysmotility and to determine the optimal management of achalasia after a LSG.
Disclosures:
Stavros Doumas, MD, MS, PhD1, Corinne O'Connor, MD1, Fredrick Brody, MD2, Marianna Papademetriou, MD2. P2299 - Is It a Wrap? Achalasia Management After Sleeve Gastrectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2Washington DC VA Medical Center, Washington, DC
Introduction: Esophageal dysmotility is an established complication following gastric bypass and banding and recently reported after laparoscopic sleeve gastrectomy (LSG). Dysphagia and associated dysmotility can range from mild to severe. Severe cases may reflect the evolution of primary achalasia or elevated intragastric pressure with aperistalsis, recently termed post-obesity esophageal dysfunction (POSED). Achalasia following-LSG constitutes a surgical challenge as the absence of the fundus prohibits the addition of a fundoplication in conjunction with a Heller myotomy. We report the case of a young female who developed achalasia following LSG.
Case Description/Methods: A 34-year-old woman with a long-standing GERD and obesity for which she underwent LSG four years prior presented with a two-month history of progressively worsening dysphagia to solids and liquids and precipitous weight loss. The patient denied dysphagia prior to surgery. She received Omeprazole empirically, without relief, and underwent an EGD, which demonstrated grade D esophagitis. Biopsies were positive for Candida, and she was started on pantoprazole and fluconazole. At two weeks follow-up, she reported persistent symptoms and underwent a repeat EGD with empiric balloon dilation of the LES (12mm to 15mm) without symptom improvement. She underwent an esophageal manometry that showed an IRP of 19.4mmHg with 100% failed esophageal motility with pan esophageal pressurization without elevated intragastric pressure, consistent with Type 2 Achalasia. The patient underwent a laparoscopic Heller Myotomy with plication of the myotomy site to the diaphragmatic crura with sutures to mimic the tension created by a fundoplication. The patient’s post-operative course was uncomplicated, and she reported significant improvement of her dysphagia.
Discussion: Severe esophageal dysmotility is increasingly recognized in patients undergoing LSG. Achalasia remains rare after bariatric surgery; however, it appears that surgery may be a risk factor. Because our patient had an elevated IRP and normal intragastric pressure, we elected to treat this patient as primary achalasia. It is currently unclear which patients are at risk of developing esophageal dysmotility. Management of achalasia in the setting of prior LSG poses a particular surgical challenge. Future studies are needed to identify the patients at risk of developing post-LSG esophageal dysmotility and to determine the optimal management of achalasia after a LSG.
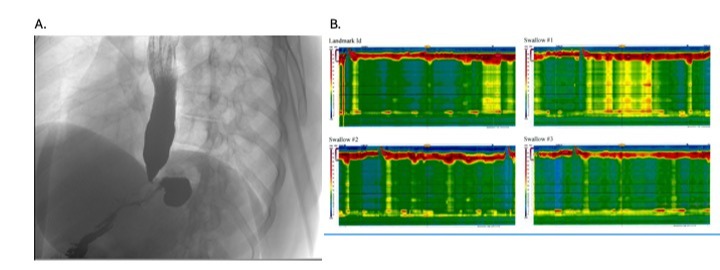
Figure: A. Esophagogram demonstrating characteristic Bird's Beak appearance B. Esophageal Manometry demonstrating 100% failed esophageal motility with pan esophageal pressurization without elevated intragastric pressure.
Disclosures:
Stavros Doumas indicated no relevant financial relationships.
Corinne O'Connor indicated no relevant financial relationships.
Fredrick Brody indicated no relevant financial relationships.
Marianna Papademetriou indicated no relevant financial relationships.
Stavros Doumas, MD, MS, PhD1, Corinne O'Connor, MD1, Fredrick Brody, MD2, Marianna Papademetriou, MD2. P2299 - Is It a Wrap? Achalasia Management After Sleeve Gastrectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
