Monday Poster Session
Category: Esophagus
P2322 - Acute Esophageal Necrosis in a COVID Positive Patient After Anti-Viral Therapy Complicated by Esophageal Stricture
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Brandon Stahl, MD
Albany Medical Center
Albany, NY
Presenting Author(s)
Brandon Stahl, MD, Anika Paradkar, MD, Peter Ells, MD
Albany Medical Center, Albany, NY
Introduction: Acute esophageal necrosis (AEN) is a rare endoscopic entity with a high mortality rate, characterized by full circumferential black tissue in the esophagus. COVID has emerged as a potential risk factor for AEN due to hypoperfusion, coagulopathies, and vasculopathies. Sequalae include esophageal stricture, perforation, and rupture and long-term management of these in AEN have not been well-defined. This case demonstrates AEN in a COVID positive patient and our long-term management strategy for their esophageal stricture.
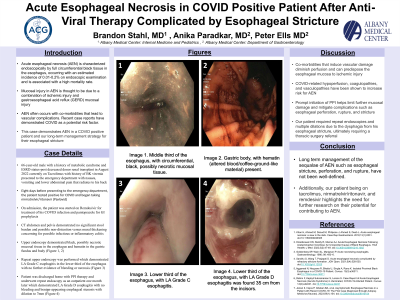
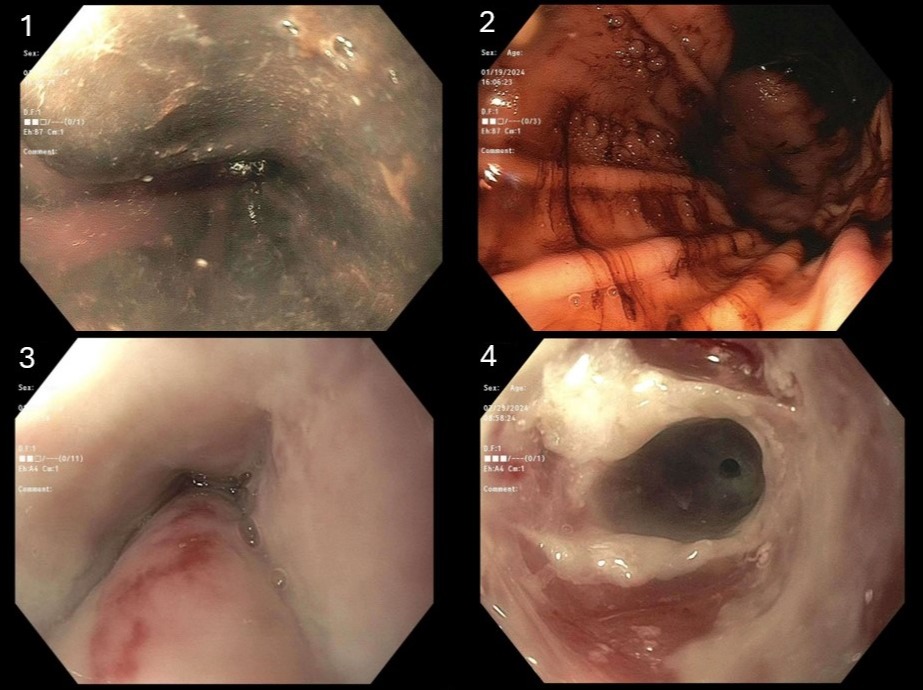
Case Description/Methods: A 66-year-old male with a history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and ESRD status-post deceased donor renal transplant currently on tacrolimus with history of BK viremia presented to the emergency department with nausea, vomiting and lower abdominal pain that radiated to his back. Eight days prior he tested positive for COVID and began taking nirmatrelvir/ritonavir and on admission was started on remdesivir. The initial CT was concerning for infectious or inflammatory colitis however a few days later developed melena. His initial EGD showed black, possibly necrotic mucosal tissue in the esophagus and hematin in the gastric fundus and body (Figure 1, 2) concerning for acute esophageal necrosis. Repeat EGD ten days later demonstrated LA Grade C esophagitis in the lower third of the esophagus without bleeding or necrosis (Figure 3). He was discharged home on daily pantoprazole and famotidine and had a repeat EGD showing LA Grade D esophagitis without bleeding and benign-appearing esophageal stenosis (Figure 4). Since then, he has had six Savary dilations as an outpatient and was referred to thoracic surgery for esophagectomy.
Discussion: Co-morbidities that induce vascular damage diminish perfusion and can predispose the esophageal mucosa to ischemic injury. Recently, COVID-related hypoperfusion, coagulopathies, and vasculopathies have been shown to increase risk for AEN. Prompt initiation of PPI helps limit further mucosal damage and mitigate complications such as esophageal perforation, rupture, and stricture. Our patient required repeat endoscopies for disease assessment and therapeutic intervention due to dysphagia with esophageal stricture. For our patient, it is unclear whether his COVID medications contributed to his AEN. Our patient being on tacrolimus, nirmatrelvir/ritonavir, and remdesivir highlights the need for further research on their potential for contributing to AEN.
Disclosures:
Brandon Stahl, MD, Anika Paradkar, MD, Peter Ells, MD. P2322 - Acute Esophageal Necrosis in a COVID Positive Patient After Anti-Viral Therapy Complicated by Esophageal Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Acute esophageal necrosis (AEN) is a rare endoscopic entity with a high mortality rate, characterized by full circumferential black tissue in the esophagus. COVID has emerged as a potential risk factor for AEN due to hypoperfusion, coagulopathies, and vasculopathies. Sequalae include esophageal stricture, perforation, and rupture and long-term management of these in AEN have not been well-defined. This case demonstrates AEN in a COVID positive patient and our long-term management strategy for their esophageal stricture.
Case Description/Methods: A 66-year-old male with a history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and ESRD status-post deceased donor renal transplant currently on tacrolimus with history of BK viremia presented to the emergency department with nausea, vomiting and lower abdominal pain that radiated to his back. Eight days prior he tested positive for COVID and began taking nirmatrelvir/ritonavir and on admission was started on remdesivir. The initial CT was concerning for infectious or inflammatory colitis however a few days later developed melena. His initial EGD showed black, possibly necrotic mucosal tissue in the esophagus and hematin in the gastric fundus and body (Figure 1, 2) concerning for acute esophageal necrosis. Repeat EGD ten days later demonstrated LA Grade C esophagitis in the lower third of the esophagus without bleeding or necrosis (Figure 3). He was discharged home on daily pantoprazole and famotidine and had a repeat EGD showing LA Grade D esophagitis without bleeding and benign-appearing esophageal stenosis (Figure 4). Since then, he has had six Savary dilations as an outpatient and was referred to thoracic surgery for esophagectomy.
Discussion: Co-morbidities that induce vascular damage diminish perfusion and can predispose the esophageal mucosa to ischemic injury. Recently, COVID-related hypoperfusion, coagulopathies, and vasculopathies have been shown to increase risk for AEN. Prompt initiation of PPI helps limit further mucosal damage and mitigate complications such as esophageal perforation, rupture, and stricture. Our patient required repeat endoscopies for disease assessment and therapeutic intervention due to dysphagia with esophageal stricture. For our patient, it is unclear whether his COVID medications contributed to his AEN. Our patient being on tacrolimus, nirmatrelvir/ritonavir, and remdesivir highlights the need for further research on their potential for contributing to AEN.
Figure: Image 1. Middle third of the esophagus, with circumferential, black, possibly necrotic mucosal tissue. Image 2. Gastric body, with hematin (altered blood/coffee-ground-like material) present. Image 3. Lower third of the esophagus, with LA Grade C esophagitis. Image 4. Lower third of the esophagus, with LA Grade D esophagitis was found 35 cm from the incisors.
Disclosures:
Brandon Stahl indicated no relevant financial relationships.
Anika Paradkar indicated no relevant financial relationships.
Peter Ells indicated no relevant financial relationships.
Brandon Stahl, MD, Anika Paradkar, MD, Peter Ells, MD. P2322 - Acute Esophageal Necrosis in a COVID Positive Patient After Anti-Viral Therapy Complicated by Esophageal Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
