Monday Poster Session
Category: Esophagus
P2325 - Recurrent Proximal Esophageal Stricture: Sequela of Lymphocytic Esophagitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- YA
Yasir Ali, MD
Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Yasir Ali, MD1, Nader Daoud, MD2, Sharanya Nemakallu, MD2, Derrick Cheung, MD2
1Brookdale University Hospital Medical Center, Brooklyn, NY; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY
Introduction: Lymphocytic esophagitis (LE) is an extremely rare disorder of mainly women in their sixth decade. Incidence reported to be 0.1% of total esophageal biopsies based on a large pilot study in the US of more than 40,000 patients. The clinical presentation of LE may include dysphagia as in our patient, dyspepsia or chest pain. Esophagogastroduodenoscopy (EGD) with biopsies is the gold standard for diagnosis which reveals increased peripapillary intraepithelial lymphocytes. We report a biopsy-proven case of LE in a 80-year old female presented with recurrent proximal esophageal stricture requiring endoscopic dilation
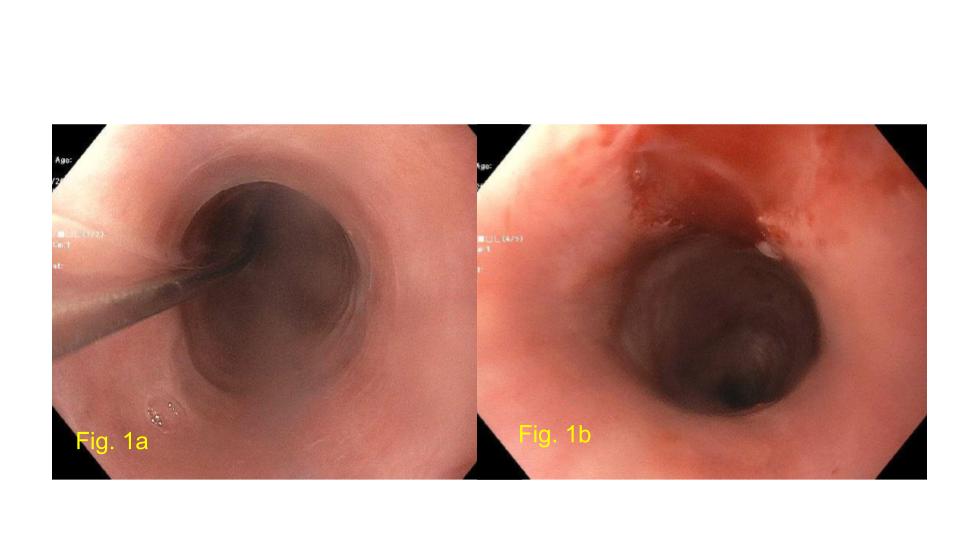
Case Description/Methods: A 80-year-old female with history of asthma, DM, HTN and dysphagia due to proximal esophageal stricture S/P EGD with Savary dilation (10/28/22) up to 12.8 mm of a 3-cm long stricture (16-19 cm from incisors), biopsies consistent with lymphocytic esophagitis. Patient was recommended high dose PPI and budesonide for 8 weeks but compliance was questionable. Patient again presented with the complains of progressive dysphagia x 6 months, intermittent, mainly with solid food. Physical exam was unremarkable. Vital signs were stable. EGD was repeated (10/18/2023) and found to have a 2-cm long stricture in the proximal esophagus (16-18 cm from the incisors) S/P Savary dilation up to 15 mm over guidewire (Fig 1 a,b). Also a few non-obstructing rings seen in the mid and distal esophagus. Biopsies again revealed lymphocytic esophagitis (acute inflammation, edema, intraepithelial and papillary lymphocytes up to 30/HPF, negative for eosinophils). Patient was recommended to start PPI 40 mg twice daily and budesonide 4 mg oral viscous slurry twice daily x 12 weeks and then to de-escalate to 1 mg daily as a maintenance dose. Upon follow up, patient confirmed taking medications as prescribed and denied any symptoms of dysphagia, odynophagia or choking sensations.
Discussion: LE is a rare subtype of chronic esophagitis with unknown etiology. It is significantly associated with underlying GERD, achalasia, tobacco use, certain allergies and medications. Our patient demonstrated none of these associations. The pathogenesis of LE is not well understood but is likely a chronic inflammatory disorder of the esophagus suggested by increased expression of CD3, CD4, and CD8 proteins by esophageal intraepithelial lymphocytes. Early recognition of this debilitating and potentially fatal illness is the key to manage the patients
Disclosures:
Yasir Ali, MD1, Nader Daoud, MD2, Sharanya Nemakallu, MD2, Derrick Cheung, MD2. P2325 - Recurrent Proximal Esophageal Stricture: Sequela of Lymphocytic Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brookdale University Hospital Medical Center, Brooklyn, NY; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY
Introduction: Lymphocytic esophagitis (LE) is an extremely rare disorder of mainly women in their sixth decade. Incidence reported to be 0.1% of total esophageal biopsies based on a large pilot study in the US of more than 40,000 patients. The clinical presentation of LE may include dysphagia as in our patient, dyspepsia or chest pain. Esophagogastroduodenoscopy (EGD) with biopsies is the gold standard for diagnosis which reveals increased peripapillary intraepithelial lymphocytes. We report a biopsy-proven case of LE in a 80-year old female presented with recurrent proximal esophageal stricture requiring endoscopic dilation
Case Description/Methods: A 80-year-old female with history of asthma, DM, HTN and dysphagia due to proximal esophageal stricture S/P EGD with Savary dilation (10/28/22) up to 12.8 mm of a 3-cm long stricture (16-19 cm from incisors), biopsies consistent with lymphocytic esophagitis. Patient was recommended high dose PPI and budesonide for 8 weeks but compliance was questionable. Patient again presented with the complains of progressive dysphagia x 6 months, intermittent, mainly with solid food. Physical exam was unremarkable. Vital signs were stable. EGD was repeated (10/18/2023) and found to have a 2-cm long stricture in the proximal esophagus (16-18 cm from the incisors) S/P Savary dilation up to 15 mm over guidewire (Fig 1 a,b). Also a few non-obstructing rings seen in the mid and distal esophagus. Biopsies again revealed lymphocytic esophagitis (acute inflammation, edema, intraepithelial and papillary lymphocytes up to 30/HPF, negative for eosinophils). Patient was recommended to start PPI 40 mg twice daily and budesonide 4 mg oral viscous slurry twice daily x 12 weeks and then to de-escalate to 1 mg daily as a maintenance dose. Upon follow up, patient confirmed taking medications as prescribed and denied any symptoms of dysphagia, odynophagia or choking sensations.
Discussion: LE is a rare subtype of chronic esophagitis with unknown etiology. It is significantly associated with underlying GERD, achalasia, tobacco use, certain allergies and medications. Our patient demonstrated none of these associations. The pathogenesis of LE is not well understood but is likely a chronic inflammatory disorder of the esophagus suggested by increased expression of CD3, CD4, and CD8 proteins by esophageal intraepithelial lymphocytes. Early recognition of this debilitating and potentially fatal illness is the key to manage the patients
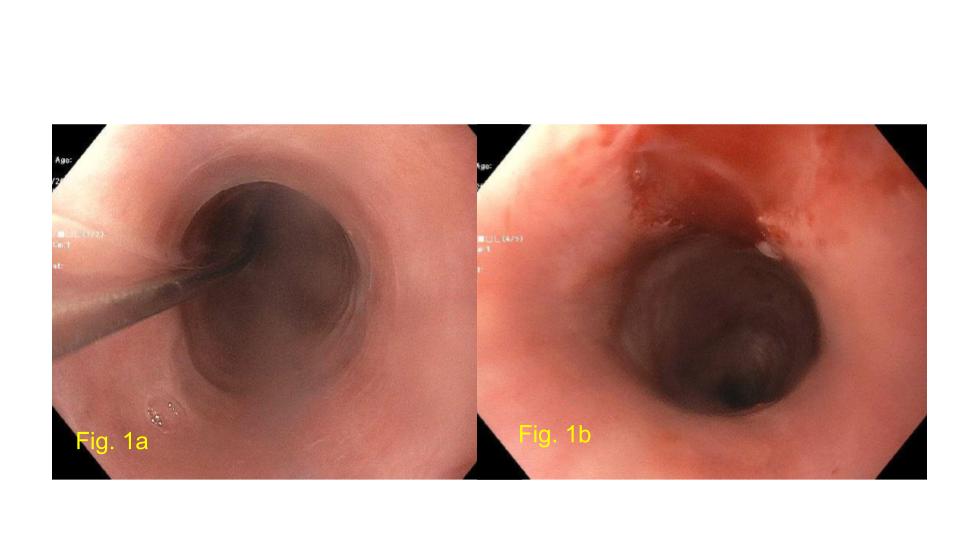
Figure: Fig 1a: S/P placement of Savary guidewire
Fig 1b: S/P Savary dilation up to 15 mm
Fig 1b: S/P Savary dilation up to 15 mm
Disclosures:
Yasir Ali indicated no relevant financial relationships.
Nader Daoud indicated no relevant financial relationships.
Sharanya Nemakallu indicated no relevant financial relationships.
Derrick Cheung indicated no relevant financial relationships.
Yasir Ali, MD1, Nader Daoud, MD2, Sharanya Nemakallu, MD2, Derrick Cheung, MD2. P2325 - Recurrent Proximal Esophageal Stricture: Sequela of Lymphocytic Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
