Monday Poster Session
Category: Esophagus
P2326 - A Snorted Story: When Cocaine Met the Esophagus
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lara Bitar, MD
McLaren Oakland Hospital
Troy, MI
Presenting Author(s)
Majd Khadra, MD1, Kenan Abou Chaer, MD1, Lara Bitar, MD2, Eduardo Gomez-Pineiro, MD1
1Detroit Medical Center/Wayne State University, Detroit, MI; 2McLaren Oakland Hospital, Pontiac, MI
Introduction: Esophagitis describes inflammation or damage to the mucosa of the esophagus. Gastroesophageal reflux is one of the most frequent causes, and it can result in erosive esophagitis. Other etiologies include radiation, infections, local injury caused by medications, pill esophagitis, substance use, and eosinophilic esophagitis.
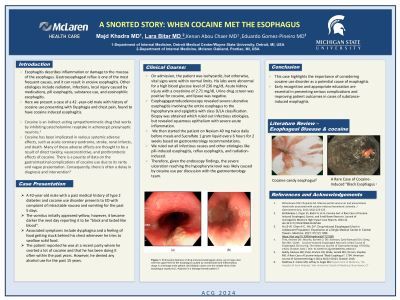
Case Description/Methods: A 42-year-old male with a past medical history of type 2 diabetes and cocaine use disorder who presented to the emergency department complaining of intractable nausea and vomiting for the past 5 days associated with dysphagia. The vomitus initially appeared yellow; however, it became darker the next day reporting it to be "black and tasted like blood". Associated symptoms include a feeling of food getting stuck behind his chest whenever he tries to swallow solid food. The patient reported he was at a recent party where he snorted a lot of cocaine and that he has been doing it often within the past years. However, he denied any alcohol use for the past 15 years. On admission, the patient was tachycardic, but otherwise, vital signs were within normal limits. His labs were abnormal for a high blood glucose level of 236 mg/dl, Acute kidney injury with a creatinine of 2.71 mg/dl, Urine drug screen was positive for cocaine, and lipase was negative. Esophagogastroduodenoscopy revealed severe ulcerative esophagitis involving the entire esophagus to the hypopharynx and epiglottis with class D/LA classification. Biopsy was obtained which ruled out infectious etiologies, but revealed squamous epithelium with severe acute inflammation. We then started the patient on Nexium 40 mg twice daily before meals and Sucralfate 1 gram liquid every 6 hours for 2 weeks based on gastroenterology recommendations. We ruled out all infectious causes and other etiologies like pill-induced esophagitis, reflux esophagitis, and radiation-induced. Therefore, given the endoscopy findings, the severe ulceration reaching the hypopharynx level was likely caused by cocaine use per discussion with the gastroenterology team.
Discussion: This case highlights the importance of considering cocaine use disorder as a potential cause of esophagitis. Early recognition and appropriate education are essential in preventing serious complications and improving patient outcomes in cases of substance-induced esophagitis.
Disclosures:
Majd Khadra, MD1, Kenan Abou Chaer, MD1, Lara Bitar, MD2, Eduardo Gomez-Pineiro, MD1. P2326 - A Snorted Story: When Cocaine Met the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2McLaren Oakland Hospital, Pontiac, MI
Introduction: Esophagitis describes inflammation or damage to the mucosa of the esophagus. Gastroesophageal reflux is one of the most frequent causes, and it can result in erosive esophagitis. Other etiologies include radiation, infections, local injury caused by medications, pill esophagitis, substance use, and eosinophilic esophagitis.
Case Description/Methods: A 42-year-old male with a past medical history of type 2 diabetes and cocaine use disorder who presented to the emergency department complaining of intractable nausea and vomiting for the past 5 days associated with dysphagia. The vomitus initially appeared yellow; however, it became darker the next day reporting it to be "black and tasted like blood". Associated symptoms include a feeling of food getting stuck behind his chest whenever he tries to swallow solid food. The patient reported he was at a recent party where he snorted a lot of cocaine and that he has been doing it often within the past years. However, he denied any alcohol use for the past 15 years. On admission, the patient was tachycardic, but otherwise, vital signs were within normal limits. His labs were abnormal for a high blood glucose level of 236 mg/dl, Acute kidney injury with a creatinine of 2.71 mg/dl, Urine drug screen was positive for cocaine, and lipase was negative. Esophagogastroduodenoscopy revealed severe ulcerative esophagitis involving the entire esophagus to the hypopharynx and epiglottis with class D/LA classification. Biopsy was obtained which ruled out infectious etiologies, but revealed squamous epithelium with severe acute inflammation. We then started the patient on Nexium 40 mg twice daily before meals and Sucralfate 1 gram liquid every 6 hours for 2 weeks based on gastroenterology recommendations. We ruled out all infectious causes and other etiologies like pill-induced esophagitis, reflux esophagitis, and radiation-induced. Therefore, given the endoscopy findings, the severe ulceration reaching the hypopharynx level was likely caused by cocaine use per discussion with the gastroenterology team.
Discussion: This case highlights the importance of considering cocaine use disorder as a potential cause of esophagitis. Early recognition and appropriate education are essential in preventing serious complications and improving patient outcomes in cases of substance-induced esophagitis.
Disclosures:
Majd Khadra indicated no relevant financial relationships.
Kenan Abou Chaer indicated no relevant financial relationships.
Lara Bitar indicated no relevant financial relationships.
Eduardo Gomez-Pineiro indicated no relevant financial relationships.
Majd Khadra, MD1, Kenan Abou Chaer, MD1, Lara Bitar, MD2, Eduardo Gomez-Pineiro, MD1. P2326 - A Snorted Story: When Cocaine Met the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
