Monday Poster Session
Category: Functional Bowel Disease
P2357 - Hormone Replacement Therapy Is Associated With Increased Risk of Developing Irritable Bowel Syndrome in Post-Menopausal Women
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jacqueline Khalil, MS, DO
Case Western Reserve University/Metro Health
Beachwood, OH
Presenting Author(s)
Award: Presidential Poster Award
Jacqueline Khalil, MS, DO1, Yan Sun, MD2, David Kaelber, MD, PhD, MPH3, Anthony J. Lembo, MD4, Gengqing Song, MD, PhD5
1Case Western Reserve University/Metro Health, Beachwood, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Case Western Reserve University/Metro Health, Cleveland, OH; 4Digestive Disease Institute, Cleveland Clinic, Cleveland, OH; 5Metrohealth Medical Center, Cleveland, OH
Introduction: IBS disproportionately affects women. Female sex hormones are hypothesized to play a significant role. This study investigated the effects of hormone replacement therapy (HRT) on IBS and its related symptoms, medication use, and diagnostic testing in post-menopausal women.
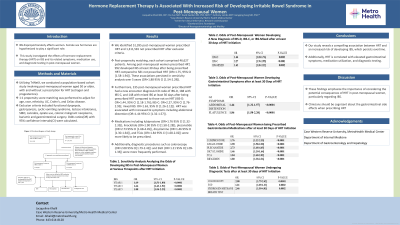
Methods: Utilizing TriNetX, we conducted a population-based cohort study involving post-menopausal women aged 50 or older, with and without a prescription for HRT (estrogen and progesterone). 1:1 propensity score matching was performed to adjust for age, race, ethnicity, UC, Crohn’s, and Celiac disease. Exclusion criteria included functional dyspepsia, gastroparesis, cyclic vomiting syndrome, lactose intolerance, SIBO, cannabis, opiate use, colonic malignant neoplasms, bariatric and gastrointestinal surgery. Odds ratios(OR) with 95% confidence intervals(CI) were calculated.
Results: We identified 51,395 post-menopausal women prescribed HRT and 1,311,581 not prescribed HRT after exclusion criteria. Post-propensity matching, each cohort comprised 46,627 patients. Among post-menopausal women prescribed HRT, 992 developed IBS at least 30 days after being prescribed HRT compared to 581 not prescribed HRT (OR=1.75, 95% CI [1.58-1.94]). These associations persisted in sensitivity analysis over 5 years (OR=1.88 95% CI [1.54-2.29]). Furthermore, 235 post-menopausal women prescribed HRT had a new encounter diagnosis ICD code of IBS-D, 188 with IBS-C, and 148 with mixed IBS at least 30 days after being prescribed HRT compared to those not on HRT (IBS-D: OR=1.44, 95% CI [1.18-1.76]; IBS-C: OR=2.27, 95% CI [1.76-2.95]; mixed IBS: OR=1.63, 95% CI [1.26-2.12]). HRT was associated with increased GI symptoms including abdominal distention (OR=1.44 95% CI [1.32-1.57]). Medications including lubiprostone (OR=1.76 95% CI [1.32-2.35]), linaclotide (OR=1.90 95% CI [1.58-2.28]), plecanatide (OR=2.73 95% CI [1.68-4.45]), dicyclomine (OR=1.46 95% CI [1.30-1.64]), and TCAs (OR=1.84 95% CI [1.68-2.02]) were more likely to be prescribed. Additionally, diagnostic procedures such as colonoscopy (OR=2.08 95% CI[1.79-2.42]) and EGD (OR=1.21 95% CI[1.09-1.33]) were more frequently performed.
Discussion: HRT is associated with an increased risk of developing IBS, which persists overtime. Additionally, HRT is correlated with elevated gastrointestinal symptoms, medication utilization, and diagnostic testing. These findings emphasize the importance of considering the potential consequences of HRT in post-menopausal women, particularly regarding IBS.
Disclosures:
Jacqueline Khalil, MS, DO1, Yan Sun, MD2, David Kaelber, MD, PhD, MPH3, Anthony J. Lembo, MD4, Gengqing Song, MD, PhD5. P2357 - Hormone Replacement Therapy Is Associated With Increased Risk of Developing Irritable Bowel Syndrome in Post-Menopausal Women, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jacqueline Khalil, MS, DO1, Yan Sun, MD2, David Kaelber, MD, PhD, MPH3, Anthony J. Lembo, MD4, Gengqing Song, MD, PhD5
1Case Western Reserve University/Metro Health, Beachwood, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Case Western Reserve University/Metro Health, Cleveland, OH; 4Digestive Disease Institute, Cleveland Clinic, Cleveland, OH; 5Metrohealth Medical Center, Cleveland, OH
Introduction: IBS disproportionately affects women. Female sex hormones are hypothesized to play a significant role. This study investigated the effects of hormone replacement therapy (HRT) on IBS and its related symptoms, medication use, and diagnostic testing in post-menopausal women.
Methods: Utilizing TriNetX, we conducted a population-based cohort study involving post-menopausal women aged 50 or older, with and without a prescription for HRT (estrogen and progesterone). 1:1 propensity score matching was performed to adjust for age, race, ethnicity, UC, Crohn’s, and Celiac disease. Exclusion criteria included functional dyspepsia, gastroparesis, cyclic vomiting syndrome, lactose intolerance, SIBO, cannabis, opiate use, colonic malignant neoplasms, bariatric and gastrointestinal surgery. Odds ratios(OR) with 95% confidence intervals(CI) were calculated.
Results: We identified 51,395 post-menopausal women prescribed HRT and 1,311,581 not prescribed HRT after exclusion criteria. Post-propensity matching, each cohort comprised 46,627 patients. Among post-menopausal women prescribed HRT, 992 developed IBS at least 30 days after being prescribed HRT compared to 581 not prescribed HRT (OR=1.75, 95% CI [1.58-1.94]). These associations persisted in sensitivity analysis over 5 years (OR=1.88 95% CI [1.54-2.29]). Furthermore, 235 post-menopausal women prescribed HRT had a new encounter diagnosis ICD code of IBS-D, 188 with IBS-C, and 148 with mixed IBS at least 30 days after being prescribed HRT compared to those not on HRT (IBS-D: OR=1.44, 95% CI [1.18-1.76]; IBS-C: OR=2.27, 95% CI [1.76-2.95]; mixed IBS: OR=1.63, 95% CI [1.26-2.12]). HRT was associated with increased GI symptoms including abdominal distention (OR=1.44 95% CI [1.32-1.57]). Medications including lubiprostone (OR=1.76 95% CI [1.32-2.35]), linaclotide (OR=1.90 95% CI [1.58-2.28]), plecanatide (OR=2.73 95% CI [1.68-4.45]), dicyclomine (OR=1.46 95% CI [1.30-1.64]), and TCAs (OR=1.84 95% CI [1.68-2.02]) were more likely to be prescribed. Additionally, diagnostic procedures such as colonoscopy (OR=2.08 95% CI[1.79-2.42]) and EGD (OR=1.21 95% CI[1.09-1.33]) were more frequently performed.
Discussion: HRT is associated with an increased risk of developing IBS, which persists overtime. Additionally, HRT is correlated with elevated gastrointestinal symptoms, medication utilization, and diagnostic testing. These findings emphasize the importance of considering the potential consequences of HRT in post-menopausal women, particularly regarding IBS.
Disclosures:
Jacqueline Khalil indicated no relevant financial relationships.
Yan Sun indicated no relevant financial relationships.
David Kaelber indicated no relevant financial relationships.
Anthony Lembo: Allurion – Stock Options. Bristol Myers Squibb – Stock Options. Johnson & Johnson – Stock Options. Vibrant Advisory Board – Advisory Committee/Board Member.
Gengqing Song indicated no relevant financial relationships.
Jacqueline Khalil, MS, DO1, Yan Sun, MD2, David Kaelber, MD, PhD, MPH3, Anthony J. Lembo, MD4, Gengqing Song, MD, PhD5. P2357 - Hormone Replacement Therapy Is Associated With Increased Risk of Developing Irritable Bowel Syndrome in Post-Menopausal Women, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


