Monday Poster Session
Category: Functional Bowel Disease
P2360 - Evaluating Trends In Rumination Syndrome: A Retrospective Analysis of El Paso Population
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shivangini Duggal, MD
TTUHSC
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Misbah Jilani, MD2, Jose W. Sotelo, MD3, Richard W. McCallum, MD4
1TTUHSC, El Paso, TX; 2Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 3Texas Tech University Health Sciences Center, El Paso, TX; 4Texas Tech University Health Sciences Center School of Medicine, El Paso, TX
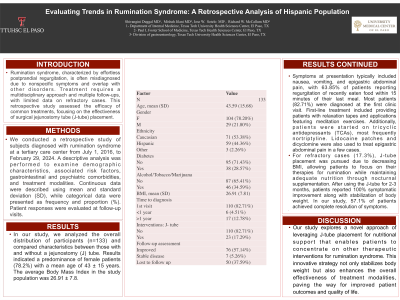
Introduction: Rumination syndrome, characterized by effortless postprandial regurgitation, is often misdiagnosed due to nonspecific symptoms and overlap with other disorders. Treatment requires a multidisciplinary approach and multiple follow-ups, with limited data on refractory cases. This retrospective study assessed the efficacy of common treatments, focusing on the effectiveness of surgical jejunostomy tube (J-tube) placement.
Methods: We conducted a retrospective study of subjects diagnosed with rumination syndrome at a tertiary care center from July 1, 2016, to February 29, 2024. A descriptive analysis was performed to examine demographic characteristics, associated risk factors, gastrointestinal and psychiatric comorbidities, and treatment modalities. Continuous data were described using mean and standard deviation (SD), while categorical data were presented as frequency and proportion (%). Patient responses were evaluated at follow-up visits.
Results: Results indicated a predominance of female patients (77.6%) with a mean age of 43 ± 15 years. The average Body Mass Index in the study population was 27.65 ± 7.8. Coexisting conditions included GERD (32.08%) and psychiatric disorders such as MDD and GAD (75%). Symptoms at presentation typically included nausea, vomiting, and epigastric abdominal pain, with 63.85% of patients reporting regurgitation of recently eaten food within 15 minutes of their last meal. Most patients (70.14%) were diagnosed at the first clinic visit. First-line treatment included providing patients with relaxation tapes and applications featuring meditation exercises. Additionally, patients were started on tricyclic antidepressants (TCAs). For refractory cases (8%), J-tube placement was pursued due to decreasing BMI, allowing patients to focus on their therapies for rumination while maintaining adequate nutrition through nocturnal supplementation. After using the J-tube for 2-3 months, patients reported 100% symptomatic improvement along with stabilization of body weight. In our study, 47.8% of patients achieved complete resolution of symptoms.
Discussion: Our study explores a novel approach of leveraging J-tube placement for nutritional support that enables patients to concentrate on other therapeutic interventions for rumination syndrome. This innovative strategy stabilizes body weight and enhances the overall effectiveness of treatment modalities, resulting in improved patient outcomes and quality of life.
Disclosures:
Shivangini Duggal, MD1, Misbah Jilani, MD2, Jose W. Sotelo, MD3, Richard W. McCallum, MD4. P2360 - Evaluating Trends In Rumination Syndrome: A Retrospective Analysis of El Paso Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TTUHSC, El Paso, TX; 2Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 3Texas Tech University Health Sciences Center, El Paso, TX; 4Texas Tech University Health Sciences Center School of Medicine, El Paso, TX
Introduction: Rumination syndrome, characterized by effortless postprandial regurgitation, is often misdiagnosed due to nonspecific symptoms and overlap with other disorders. Treatment requires a multidisciplinary approach and multiple follow-ups, with limited data on refractory cases. This retrospective study assessed the efficacy of common treatments, focusing on the effectiveness of surgical jejunostomy tube (J-tube) placement.
Methods: We conducted a retrospective study of subjects diagnosed with rumination syndrome at a tertiary care center from July 1, 2016, to February 29, 2024. A descriptive analysis was performed to examine demographic characteristics, associated risk factors, gastrointestinal and psychiatric comorbidities, and treatment modalities. Continuous data were described using mean and standard deviation (SD), while categorical data were presented as frequency and proportion (%). Patient responses were evaluated at follow-up visits.
Results: Results indicated a predominance of female patients (77.6%) with a mean age of 43 ± 15 years. The average Body Mass Index in the study population was 27.65 ± 7.8. Coexisting conditions included GERD (32.08%) and psychiatric disorders such as MDD and GAD (75%). Symptoms at presentation typically included nausea, vomiting, and epigastric abdominal pain, with 63.85% of patients reporting regurgitation of recently eaten food within 15 minutes of their last meal. Most patients (70.14%) were diagnosed at the first clinic visit. First-line treatment included providing patients with relaxation tapes and applications featuring meditation exercises. Additionally, patients were started on tricyclic antidepressants (TCAs). For refractory cases (8%), J-tube placement was pursued due to decreasing BMI, allowing patients to focus on their therapies for rumination while maintaining adequate nutrition through nocturnal supplementation. After using the J-tube for 2-3 months, patients reported 100% symptomatic improvement along with stabilization of body weight. In our study, 47.8% of patients achieved complete resolution of symptoms.
Discussion: Our study explores a novel approach of leveraging J-tube placement for nutritional support that enables patients to concentrate on other therapeutic interventions for rumination syndrome. This innovative strategy stabilizes body weight and enhances the overall effectiveness of treatment modalities, resulting in improved patient outcomes and quality of life.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Misbah Jilani indicated no relevant financial relationships.
Jose Sotelo indicated no relevant financial relationships.
Richard McCallum: Evoke Pharma – Consultant.
Shivangini Duggal, MD1, Misbah Jilani, MD2, Jose W. Sotelo, MD3, Richard W. McCallum, MD4. P2360 - Evaluating Trends In Rumination Syndrome: A Retrospective Analysis of El Paso Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
