Monday Poster Session
Category: General Endoscopy
P2401 - Balancing Benefits and Risks: Evaluating Tranexamic Acid for Management of Acute GI Bleeding - A Systematic Review and Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Yash R. Shah, MD
Trinity Health Oakland / Wayne State University School of Medicine
Pontiac, MI
Presenting Author(s)
Yash R. Shah, MD1, Ernesto Calderon-Martinez, MD2, Fides Myles C. Caliwag, MD, MBA3, Nathnael Abera Woldehana, MD4, Gabriela Briceno Silva, MD5, Rodrigo Sebastian Maldonado, MD6, Nabin Khadka, MD7, Rubeliz Bolivar-Barrios, MD8, Charmy Parikh, MD9, Mihir P. Shah, MD10, Raj H. Patel, MD11, Rashmi Advani, MD12
1Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 2University of Texas at Houston, Houston, TX; 3Ateneo School of Medicine and Public Health, Pasig, National Capital Region, Philippines; 4Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 5Universidad de Oriente, Cumana, Sucre, Venezuela; 6Universidad Nacional de Cordoba, Cordoba, Cordoba, Argentina; 7Virgen Milagrosa University Foundation, San Carlos, Pangasinan, Philippines; 8Universidad de Oriente, Puerto La Cruz, Anzoategui, Venezuela; 9Mercy Catholic Medical Center, Darby, PA; 10John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 11St. Mary Medical Center, Bensalem, PA; 12Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Gastrointestinal (GI) bleeding is a prevalent medical emergency, causing substantial hospitalizations globally. Mortality remains high (2.4-11%) despite therapeutic advancements. Tranexamic acid (TXA), an antifibrinolytic medication, has been proposed to reduce bleeding by inhibiting clot breakdown. However, the HALT-IT trial raised questions about efficacy and safety, showing no mortality reduction and potential thromboembolic complications. This meta-analysis evaluates TXA's effectiveness and safety in treating acute GI bleeding.
Methods: This systematic review and meta-analysis adhered to PRISMA 2020 guidelines. A comprehensive literature search using relevant MeSH terms and keywords for TXA and GI bleeding was conducted across PubMed, ICTRP,ClinicalTrials.gov, Web of Science, Google Scholar, CINAHL, Cochrane Library, EMBASE, Scopus, LILACS, and CNKI databases (search date: March 29, 2024). We focused on patients with acute GI bleeding receiving TXA compared to placebo or standard treatment. Primary outcomes measured included mortality, blood transfusion requirements, surgical intervention need,and thromboembolic events. Randomized controlled trials (RCTs) and observational studies in English or Spanish were included.
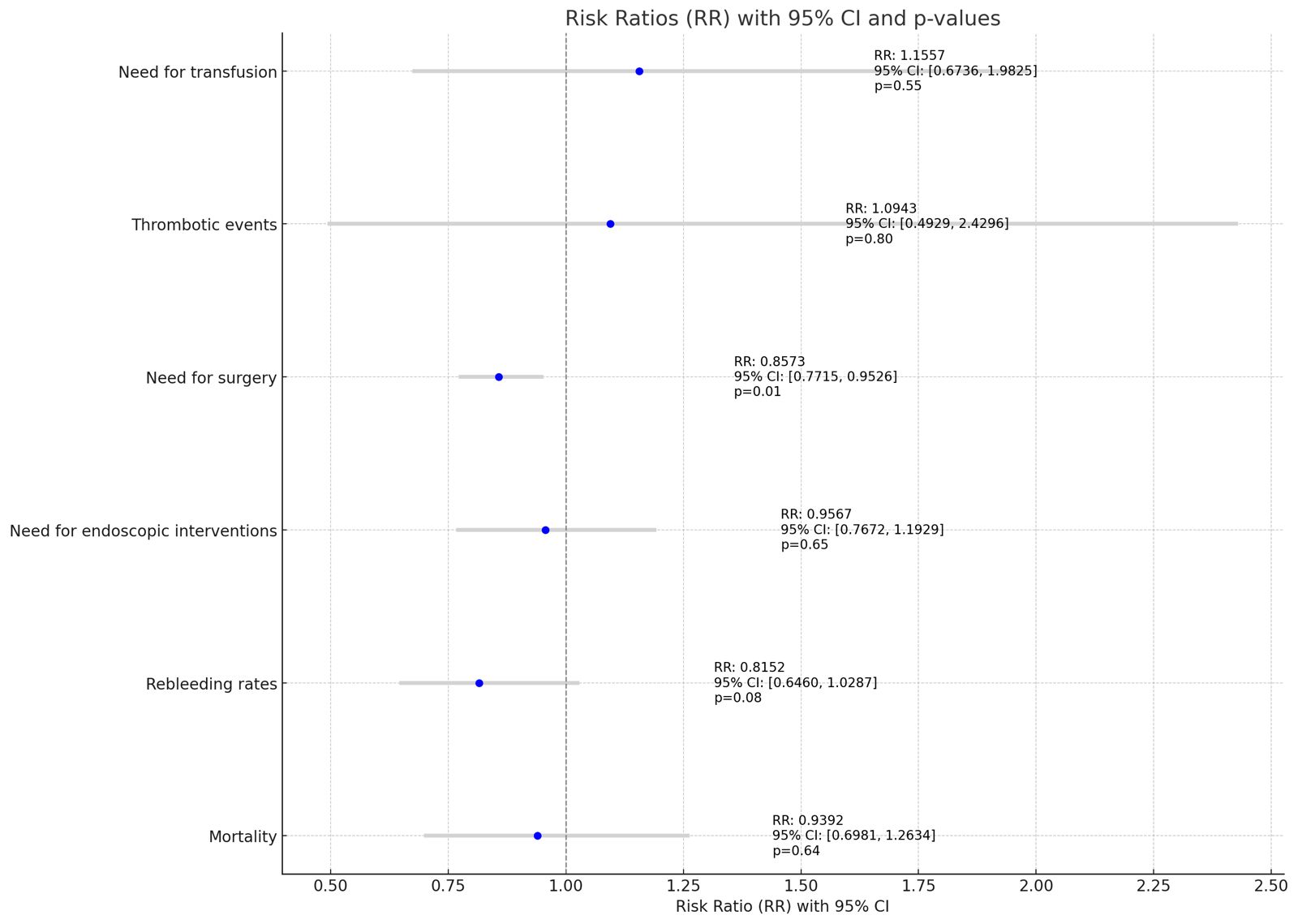
Results: The search yielded 6,810 articles. After title and abstract screening, 77 articles underwent full-text review, and 17 studies (totaling 2,059,147 participants) met the inclusion criteria. The meta-analysis revealed no significant increase in blood transfusion needs (RR 1.15, 95% CI: 0.67-1.98) with TXA. There was a trend towards increased thrombotic events in the TXA group (RR 1.09, 95% CI: 0.49-2.43), however, it did not reach statistical significance. TXA use reduced the need for surgical intervention (RR 0.86, 95% CI: 0.77-0.95) but showed no significant impact on mortality (RR 0.9392, 95% CI:0.6981-1.2634), endoscopic interventions (RR0.95, 95% CI:0.76,1.19), and rebleeding rates (RR: 0.81, 95% CI: 0.64-1.02). (Figure 1).
Discussion: TXA may decrease rebleeding and transfusion needs in acute GI bleeding, but its use carries potential risks like thromboembolic events. Further large-scale, well-designed RCTs are crucial to confirm TXA's efficacy and safety in this context. Conflicting results necessitate cautious interpretation and individualized patient management when considering TXA for GI bleeding.
Disclosures:
Yash R. Shah, MD1, Ernesto Calderon-Martinez, MD2, Fides Myles C. Caliwag, MD, MBA3, Nathnael Abera Woldehana, MD4, Gabriela Briceno Silva, MD5, Rodrigo Sebastian Maldonado, MD6, Nabin Khadka, MD7, Rubeliz Bolivar-Barrios, MD8, Charmy Parikh, MD9, Mihir P. Shah, MD10, Raj H. Patel, MD11, Rashmi Advani, MD12. P2401 - Balancing Benefits and Risks: Evaluating Tranexamic Acid for Management of Acute GI Bleeding - A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 2University of Texas at Houston, Houston, TX; 3Ateneo School of Medicine and Public Health, Pasig, National Capital Region, Philippines; 4Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 5Universidad de Oriente, Cumana, Sucre, Venezuela; 6Universidad Nacional de Cordoba, Cordoba, Cordoba, Argentina; 7Virgen Milagrosa University Foundation, San Carlos, Pangasinan, Philippines; 8Universidad de Oriente, Puerto La Cruz, Anzoategui, Venezuela; 9Mercy Catholic Medical Center, Darby, PA; 10John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 11St. Mary Medical Center, Bensalem, PA; 12Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Gastrointestinal (GI) bleeding is a prevalent medical emergency, causing substantial hospitalizations globally. Mortality remains high (2.4-11%) despite therapeutic advancements. Tranexamic acid (TXA), an antifibrinolytic medication, has been proposed to reduce bleeding by inhibiting clot breakdown. However, the HALT-IT trial raised questions about efficacy and safety, showing no mortality reduction and potential thromboembolic complications. This meta-analysis evaluates TXA's effectiveness and safety in treating acute GI bleeding.
Methods: This systematic review and meta-analysis adhered to PRISMA 2020 guidelines. A comprehensive literature search using relevant MeSH terms and keywords for TXA and GI bleeding was conducted across PubMed, ICTRP,ClinicalTrials.gov, Web of Science, Google Scholar, CINAHL, Cochrane Library, EMBASE, Scopus, LILACS, and CNKI databases (search date: March 29, 2024). We focused on patients with acute GI bleeding receiving TXA compared to placebo or standard treatment. Primary outcomes measured included mortality, blood transfusion requirements, surgical intervention need,and thromboembolic events. Randomized controlled trials (RCTs) and observational studies in English or Spanish were included.
Results: The search yielded 6,810 articles. After title and abstract screening, 77 articles underwent full-text review, and 17 studies (totaling 2,059,147 participants) met the inclusion criteria. The meta-analysis revealed no significant increase in blood transfusion needs (RR 1.15, 95% CI: 0.67-1.98) with TXA. There was a trend towards increased thrombotic events in the TXA group (RR 1.09, 95% CI: 0.49-2.43), however, it did not reach statistical significance. TXA use reduced the need for surgical intervention (RR 0.86, 95% CI: 0.77-0.95) but showed no significant impact on mortality (RR 0.9392, 95% CI:0.6981-1.2634), endoscopic interventions (RR0.95, 95% CI:0.76,1.19), and rebleeding rates (RR: 0.81, 95% CI: 0.64-1.02). (Figure 1).
Discussion: TXA may decrease rebleeding and transfusion needs in acute GI bleeding, but its use carries potential risks like thromboembolic events. Further large-scale, well-designed RCTs are crucial to confirm TXA's efficacy and safety in this context. Conflicting results necessitate cautious interpretation and individualized patient management when considering TXA for GI bleeding.
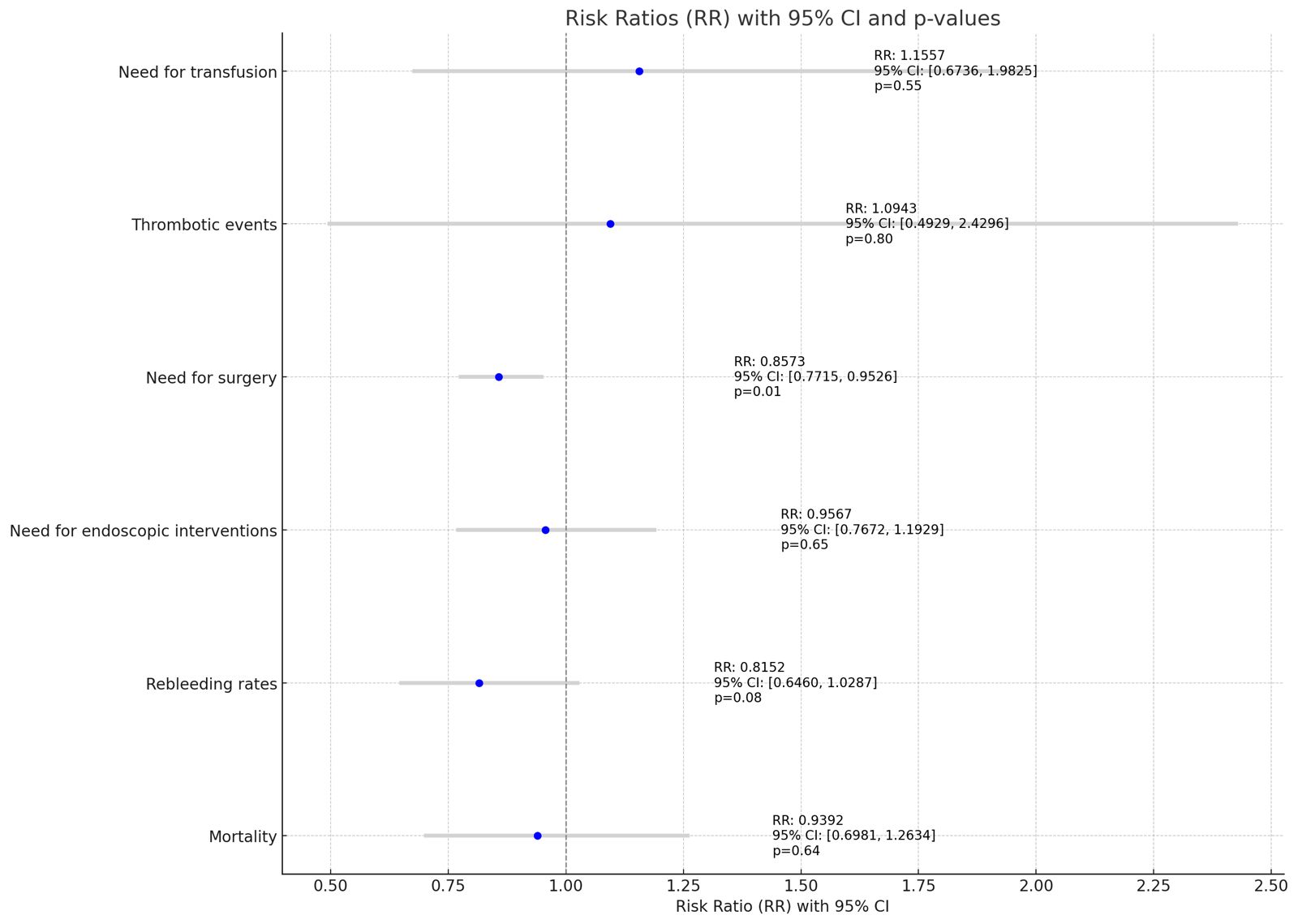
Figure: Figure 1: Outcomes of Tranexamic Acid in Management of Acute GI Bleed
Disclosures:
Yash Shah indicated no relevant financial relationships.
Ernesto Calderon-Martinez indicated no relevant financial relationships.
Fides Myles C. Caliwag indicated no relevant financial relationships.
Nathnael Abera Woldehana indicated no relevant financial relationships.
Gabriela Briceno Silva indicated no relevant financial relationships.
Rodrigo Sebastian Maldonado indicated no relevant financial relationships.
Nabin Khadka indicated no relevant financial relationships.
Rubeliz Bolivar-Barrios indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Mihir Shah indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Yash R. Shah, MD1, Ernesto Calderon-Martinez, MD2, Fides Myles C. Caliwag, MD, MBA3, Nathnael Abera Woldehana, MD4, Gabriela Briceno Silva, MD5, Rodrigo Sebastian Maldonado, MD6, Nabin Khadka, MD7, Rubeliz Bolivar-Barrios, MD8, Charmy Parikh, MD9, Mihir P. Shah, MD10, Raj H. Patel, MD11, Rashmi Advani, MD12. P2401 - Balancing Benefits and Risks: Evaluating Tranexamic Acid for Management of Acute GI Bleeding - A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
