Monday Poster Session
Category: General Endoscopy
P2408 - Safety and Efficacy of Overtube-Assisted Percutaneous Gastrostomy Tube Placement in Patients With Head and Neck Cancer: A Case Series
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Sneha Saha, MD
Yale University School of Medicine
New Haven, CT
Presenting Author(s)
Sneha Saha, MD1, Gyanprakash Ketwaroo, MD2, Amy Ogurick, MD3, Basile Njei, MD4, Petr Protiva, MD, MPH3
1Yale University School of Medicine and VA Connecticut Heathcare System, West Haven, CT; 2Yale Digestive Diseases and VA Connecticut Halthcare System, West Haven, CT; 3Yale Digestive Diseases and VA Connecticut Healthcare System, West Haven, CT; 4Yale University School of Medicine, New Haven, CT
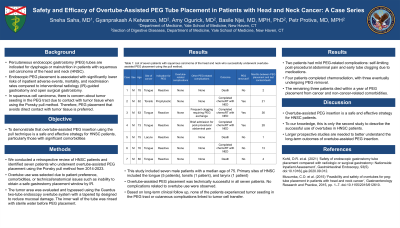
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are used for dysphagia or malnutrition in patients with squamous cell carcinoma of the head and neck (HNSC). Endoscopic PEG placement has lower risks of inpatient adverse events, mortality, and readmission rates compared to interventional radiology (IR)-guided and open surgical gastrostomy. However, there's concern about tumor seeding in the PEG tract due to contact with tumor tissue using the Ponsky pull method, so a technique avoiding direct tumor contact is preferred.
Case Description/Methods: We retrospectively reviewed HNSC patients and identified seven who underwent successful overtube-assisted PEG placement using the Ponsky pull method between 2014 and 2023. All patients had non-obstructing tumors. Overtube use was due to patient preference, comorbidities, or technical/anatomical issues like the inability to obtain a safe gastrostomy placement window by radiology. The tumor area was evaluated and bypassed using the Guardus two-tube endoscopy overtube system with a tapered tip to reduce mucosal damage. The inner wall of the tube was rinsed with sterile water before PEG placement. PEG tubes were placed reactively in six patients and prophylactically in one.
The study included seven male patients with a median age of 75. Primary sites of HNSC included the tongue (5 patients), tonsils (1 patient), and larynx (1 patient). Overtube-assisted PEG placement was technically successful in all patients. Based on a median follow-up of 13 months, there was no evidence of tumor seeding in the PEG tract or cutaneous complications linked to tumor cell transfer. Two patients had mild PEG-related complications: self-limiting post-procedural abdominal pain and early tube clogging due to medications. No complications related to overtube use were observed. Four patients completed chemoradiation, with three eventually undergoing PEG removal. The remaining three patients died within a year of PEG placement from cancer and non-cancer-related comorbidities (TABLE).
Discussion: Overtube-assisted PEG insertion is a safe and effective strategy for HNSC patients. This is only the second study to describe successful overtube use in HNSC patients. Larger prospective studies are needed to better understand the long-term outcomes of overtube-assisted PEG insertion.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sneha Saha, MD1, Gyanprakash Ketwaroo, MD2, Amy Ogurick, MD3, Basile Njei, MD4, Petr Protiva, MD, MPH3. P2408 - Safety and Efficacy of Overtube-Assisted Percutaneous Gastrostomy Tube Placement in Patients With Head and Neck Cancer: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale University School of Medicine and VA Connecticut Heathcare System, West Haven, CT; 2Yale Digestive Diseases and VA Connecticut Halthcare System, West Haven, CT; 3Yale Digestive Diseases and VA Connecticut Healthcare System, West Haven, CT; 4Yale University School of Medicine, New Haven, CT
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are used for dysphagia or malnutrition in patients with squamous cell carcinoma of the head and neck (HNSC). Endoscopic PEG placement has lower risks of inpatient adverse events, mortality, and readmission rates compared to interventional radiology (IR)-guided and open surgical gastrostomy. However, there's concern about tumor seeding in the PEG tract due to contact with tumor tissue using the Ponsky pull method, so a technique avoiding direct tumor contact is preferred.
Case Description/Methods: We retrospectively reviewed HNSC patients and identified seven who underwent successful overtube-assisted PEG placement using the Ponsky pull method between 2014 and 2023. All patients had non-obstructing tumors. Overtube use was due to patient preference, comorbidities, or technical/anatomical issues like the inability to obtain a safe gastrostomy placement window by radiology. The tumor area was evaluated and bypassed using the Guardus two-tube endoscopy overtube system with a tapered tip to reduce mucosal damage. The inner wall of the tube was rinsed with sterile water before PEG placement. PEG tubes were placed reactively in six patients and prophylactically in one.
The study included seven male patients with a median age of 75. Primary sites of HNSC included the tongue (5 patients), tonsils (1 patient), and larynx (1 patient). Overtube-assisted PEG placement was technically successful in all patients. Based on a median follow-up of 13 months, there was no evidence of tumor seeding in the PEG tract or cutaneous complications linked to tumor cell transfer. Two patients had mild PEG-related complications: self-limiting post-procedural abdominal pain and early tube clogging due to medications. No complications related to overtube use were observed. Four patients completed chemoradiation, with three eventually undergoing PEG removal. The remaining three patients died within a year of PEG placement from cancer and non-cancer-related comorbidities (TABLE).
Discussion: Overtube-assisted PEG insertion is a safe and effective strategy for HNSC patients. This is only the second study to describe successful overtube use in HNSC patients. Larger prospective studies are needed to better understand the long-term outcomes of overtube-assisted PEG insertion.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sneha Saha indicated no relevant financial relationships.
Gyanprakash Ketwaroo indicated no relevant financial relationships.
Amy Ogurick indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Petr Protiva indicated no relevant financial relationships.
Sneha Saha, MD1, Gyanprakash Ketwaroo, MD2, Amy Ogurick, MD3, Basile Njei, MD4, Petr Protiva, MD, MPH3. P2408 - Safety and Efficacy of Overtube-Assisted Percutaneous Gastrostomy Tube Placement in Patients With Head and Neck Cancer: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
