Monday Poster Session
Category: General Endoscopy
P2413 - Hiding in Plain Sight: A Case of an Undiagnosed Gastrogastric Fistula in a Patient With a Remote History of Roux-en-Y Gastric Bypass
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SP
Sarmad Pirzada, MD
Trinity Health Livonia Hospital
Farmington Hills, MI
Presenting Author(s)
Sarmad Pirzada, MD1, Stefan Odabasic, MD2, Alan Putrus, MD3
1Trinity Health Livonia Hospital, Farmington Hills, MI; 2Trinity Health Livonia Hospital, Livonia, MI; 3Consultants in Digestive Health, Livonia, MI
Introduction: Gastrogastric fistula (GGF) is a rare but significant complication of Roux-en-Y gastric bypass surgery, characterized by an abnormal connection between the proximal gastric pouch and the distal gastric remnant. Occurring in up to 6% of cases, GGF can stem from technical challenges during pouch creation or post-staple-line failure, leading to abscess formation and subsequent fistula development. Recognizing and effectively managing GGF is crucial for improving patient outcomes and optimizing postoperative care.
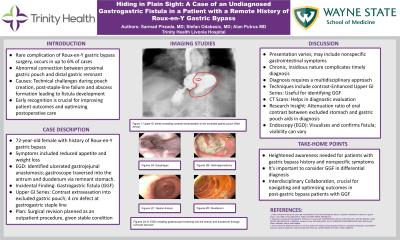
Case Description/Methods: 72-year-old female with a history of Roux-en-Y gastric bypass presented with symptoms including reduced appetite, weight loss, and hematemesis. Vital signs were stable, hemoglobin was at baseline, CT scan of the abdomen and pelvis showed no acute findings. Previous esophagogastroduodenoscopy (EGD) four years prior revealed a sizable gastric ulcer at the gastrojejunal anastomosis, necessitating clipping. A subsequent EGD one year ago noted a similar ulcer but did not require treatment. EGD during this admission identified LA grade D reflux esophagitis and an ulcerated gastrojejunal anastomosis and the gastroscope traversed into the antrum and duodenum through the remnant stomach, revealing an incidental finding of a GGF. Upper gastrointestinal series demonstrated contrast extravasation into the excluded gastric pouch, revealing a 4 cm defect at the gastrogastric staple line. Given her stable condition, surgical revision was planned as an outpatient procedure.
Discussion: GGF following gastric bypass surgery presents variably, sometimes with nonspecific gastrointestinal symptoms, complicating timely diagnosis. The condition's chronic and insidious nature contributes to diagnostic challenges for both patients and healthcare providers. Diagnosis typically involves a multidisciplinary approach integrating contrast-enhanced upper gastrointestinal series and CT scans. Research highlights the relative attenuation ratio of oral contrast in the excluded stomach to the gastric pouch as a diagnostic tool for GGF identification. Endoscopic procedures like EGD are instrumental in visualizing and confirming the fistula, though visibility may vary. This case underscores the importance of maintaining a heightened suspicion in patients with a history of gastric bypass surgery and nonspecific symptoms suggestive of GGF. Interdisciplinary collaboration is essential to navigate and optimize outcomes in patients post-gastric bypass surgery affected by this challenging condition.

Disclosures:
Sarmad Pirzada, MD1, Stefan Odabasic, MD2, Alan Putrus, MD3. P2413 - Hiding in Plain Sight: A Case of an Undiagnosed Gastrogastric Fistula in a Patient With a Remote History of Roux-en-Y Gastric Bypass, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Trinity Health Livonia Hospital, Farmington Hills, MI; 2Trinity Health Livonia Hospital, Livonia, MI; 3Consultants in Digestive Health, Livonia, MI
Introduction: Gastrogastric fistula (GGF) is a rare but significant complication of Roux-en-Y gastric bypass surgery, characterized by an abnormal connection between the proximal gastric pouch and the distal gastric remnant. Occurring in up to 6% of cases, GGF can stem from technical challenges during pouch creation or post-staple-line failure, leading to abscess formation and subsequent fistula development. Recognizing and effectively managing GGF is crucial for improving patient outcomes and optimizing postoperative care.
Case Description/Methods: 72-year-old female with a history of Roux-en-Y gastric bypass presented with symptoms including reduced appetite, weight loss, and hematemesis. Vital signs were stable, hemoglobin was at baseline, CT scan of the abdomen and pelvis showed no acute findings. Previous esophagogastroduodenoscopy (EGD) four years prior revealed a sizable gastric ulcer at the gastrojejunal anastomosis, necessitating clipping. A subsequent EGD one year ago noted a similar ulcer but did not require treatment. EGD during this admission identified LA grade D reflux esophagitis and an ulcerated gastrojejunal anastomosis and the gastroscope traversed into the antrum and duodenum through the remnant stomach, revealing an incidental finding of a GGF. Upper gastrointestinal series demonstrated contrast extravasation into the excluded gastric pouch, revealing a 4 cm defect at the gastrogastric staple line. Given her stable condition, surgical revision was planned as an outpatient procedure.
Discussion: GGF following gastric bypass surgery presents variably, sometimes with nonspecific gastrointestinal symptoms, complicating timely diagnosis. The condition's chronic and insidious nature contributes to diagnostic challenges for both patients and healthcare providers. Diagnosis typically involves a multidisciplinary approach integrating contrast-enhanced upper gastrointestinal series and CT scans. Research highlights the relative attenuation ratio of oral contrast in the excluded stomach to the gastric pouch as a diagnostic tool for GGF identification. Endoscopic procedures like EGD are instrumental in visualizing and confirming the fistula, though visibility may vary. This case underscores the importance of maintaining a heightened suspicion in patients with a history of gastric bypass surgery and nonspecific symptoms suggestive of GGF. Interdisciplinary collaboration is essential to navigate and optimize outcomes in patients post-gastric bypass surgery affected by this challenging condition.

Figure: Upper GI series revealing contrast extravasation into the excluded gastric pouch.
Disclosures:
Sarmad Pirzada indicated no relevant financial relationships.
Stefan Odabasic indicated no relevant financial relationships.
Alan Putrus indicated no relevant financial relationships.
Sarmad Pirzada, MD1, Stefan Odabasic, MD2, Alan Putrus, MD3. P2413 - Hiding in Plain Sight: A Case of an Undiagnosed Gastrogastric Fistula in a Patient With a Remote History of Roux-en-Y Gastric Bypass, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
