Monday Poster Session
Category: General Endoscopy
P2415 - Gastrocutaneous Fistula Secondary to Large Marginal Ulcer
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DS
Daniel Staursky, DO
Medical College of Georgia
Augusta, GA
Presenting Author(s)
Daniel Staursky, DO1, Amit Hudgi, MD2, Raguraj Chandradevan, MBBS2, Ahmad Alkaddour, MD2, Humberto Sifuentes, MD3
1Medical College of Georgia, Augusta, GA; 2Medical College of Georgia at Augusta University, Augusta, GA; 3Augusta University, Augusta, GA
Introduction: Marginal ulcers are a serious post operative complication in bariatric surgical patients. Late marginal ulcers are usually caused by tobacco/nonsteroidal anti-inflammatory drug (NSAID) use, H. pylori infections or other excess acid exposure to the gastric pouch. These ulcers place patients at risk for bleeding, stomal stenosis, perforation, and fistula formation. Endoscopy is frequently used for confirmatory diagnosis of marginal ulcers and their subsequent complications.
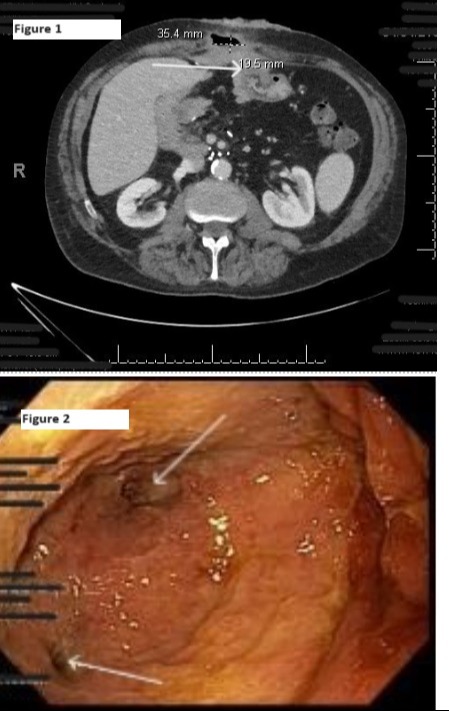
Case Description/Methods: A 66-year-old male with past medical history of with benign pancreatic disease s/p Whipple and cholecystectomy in 2010, prior duodenal ulcer in 2016, gastroesophageal reflux, and tobacco use presented as a transfer from an outside hospital for nausea, vomiting, and acute on chronic abdominal pain. He endorsed chronic abdominal pain since his Whipple procedure that acutely worsened over the past few days. Further history obtained found chronic NSAID and tobacco use for years after the Whipple procedure. Localized erythema and swelling were noted on the abdomen. Incision and drainage were performed showing necrotic skin and bilious fluid drainage. IV Zosyn and pantoprazole started, an ostomy bag was placed over the site and the patient was transferred for further surgical evaluation. CT of the abdomen found an anterior marginal ulcer with enterocutaneous fistula noted at gastrojejunal anastomosis (Figure 1). GI was consulted and EGD was notable for a large clean-based, non-bleeding ulceration with 2 fistulous openings at the GJ anastomosis (Figure 2). The fistulous site was ultimately not conducive for stent placement and ulceration was not conducive for endoscopic clip placement. Exploratory laparotomy was required which found two gastrocutaneous fistulae, a large erosive marginal ulcer, and liver to anterior abdominal wall adhesions. Ultimately, lysis of adhesions, distal gastrectomy, and Roux-en-Y reconstruction were required along with initiation of total parental nutrition.
Discussion: This case highlights the complexity with which marginal ulcers and their complications can present. Ultimately the location of the two fistulous sites were not conducive to stent placement and the ulcerated mucosa did not allow for clip placement. This chronic ulcer led to significant fistula formation and demonstrates a more indolent and chronic presentation of a marginal ulcer and its consequences. Fistulas secondary to marginal ulcers can at times be managed with endoscopy but may require surgical intervention.
Disclosures:
Daniel Staursky, DO1, Amit Hudgi, MD2, Raguraj Chandradevan, MBBS2, Ahmad Alkaddour, MD2, Humberto Sifuentes, MD3. P2415 - Gastrocutaneous Fistula Secondary to Large Marginal Ulcer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Georgia, Augusta, GA; 2Medical College of Georgia at Augusta University, Augusta, GA; 3Augusta University, Augusta, GA
Introduction: Marginal ulcers are a serious post operative complication in bariatric surgical patients. Late marginal ulcers are usually caused by tobacco/nonsteroidal anti-inflammatory drug (NSAID) use, H. pylori infections or other excess acid exposure to the gastric pouch. These ulcers place patients at risk for bleeding, stomal stenosis, perforation, and fistula formation. Endoscopy is frequently used for confirmatory diagnosis of marginal ulcers and their subsequent complications.
Case Description/Methods: A 66-year-old male with past medical history of with benign pancreatic disease s/p Whipple and cholecystectomy in 2010, prior duodenal ulcer in 2016, gastroesophageal reflux, and tobacco use presented as a transfer from an outside hospital for nausea, vomiting, and acute on chronic abdominal pain. He endorsed chronic abdominal pain since his Whipple procedure that acutely worsened over the past few days. Further history obtained found chronic NSAID and tobacco use for years after the Whipple procedure. Localized erythema and swelling were noted on the abdomen. Incision and drainage were performed showing necrotic skin and bilious fluid drainage. IV Zosyn and pantoprazole started, an ostomy bag was placed over the site and the patient was transferred for further surgical evaluation. CT of the abdomen found an anterior marginal ulcer with enterocutaneous fistula noted at gastrojejunal anastomosis (Figure 1). GI was consulted and EGD was notable for a large clean-based, non-bleeding ulceration with 2 fistulous openings at the GJ anastomosis (Figure 2). The fistulous site was ultimately not conducive for stent placement and ulceration was not conducive for endoscopic clip placement. Exploratory laparotomy was required which found two gastrocutaneous fistulae, a large erosive marginal ulcer, and liver to anterior abdominal wall adhesions. Ultimately, lysis of adhesions, distal gastrectomy, and Roux-en-Y reconstruction were required along with initiation of total parental nutrition.
Discussion: This case highlights the complexity with which marginal ulcers and their complications can present. Ultimately the location of the two fistulous sites were not conducive to stent placement and the ulcerated mucosa did not allow for clip placement. This chronic ulcer led to significant fistula formation and demonstrates a more indolent and chronic presentation of a marginal ulcer and its consequences. Fistulas secondary to marginal ulcers can at times be managed with endoscopy but may require surgical intervention.
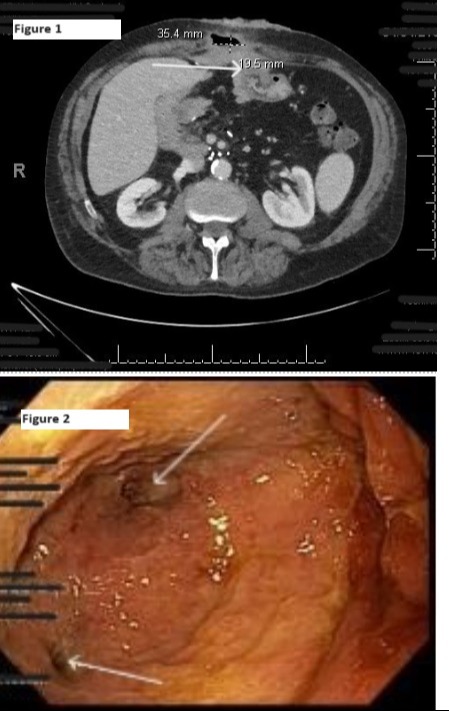
Figure: Figure 1: CT abdomen with arrow showing enterocutaneous fistula. Figure 2: Endoscopic imaging of ulceration and arrow showing fistulae
Disclosures:
Daniel Staursky indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Raguraj Chandradevan indicated no relevant financial relationships.
Ahmad Alkaddour indicated no relevant financial relationships.
Humberto Sifuentes indicated no relevant financial relationships.
Daniel Staursky, DO1, Amit Hudgi, MD2, Raguraj Chandradevan, MBBS2, Ahmad Alkaddour, MD2, Humberto Sifuentes, MD3. P2415 - Gastrocutaneous Fistula Secondary to Large Marginal Ulcer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
