Monday Poster Session
Category: GI Bleeding
P2481 - Bridge to Destruction: Rare Case of Arterio-Enteric Fistula Within an Ileal Conduit
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Saria Adnan Sultan, DO
Franciscan Health Olympia Fields
Chicago, IL
Presenting Author(s)
Saria Adnan Sultan, DO1, Saadia Jabbar, MD2, Navin Naik, DO3, Nabiha Haider, DO1, Nick Baur, DO4, Alex Yarbrough, DO1
1Franciscan Health Olympia Fields, Chicago, IL; 2Franciscan Health Olympia Fields, Homewood, IL; 3Franciscan Health Olympia Fields, Tinley Park, IL; 4Franciscan Health Olympia Fields, Olympia Fields, IL
Introduction: Gastrointestinal (GI) bleeding can turn into a serious life threatening emergency. A rare etiology is an arterio-enteric fistula (AEF) which is an abnormal connection between an artery and the GI tract. Though it only has an incidence of up to 0.07%, it carries a 50% operative mortality. Common risk factors include pelvic surgery, previous aortic or arterial surgical manipulation, and pelvic malignancy. They can be further categorized as primary or secondary. Primary causes include trauma, radiation, tumor invasion, or atherosclerotic aneurysm; while secondary AEFs typically develop after surgical intervention. We present a rare case, with no previous reports in literature, of a right external iliac to enteric fistula within an ileal conduit.
Case Description/Methods: A 65 year old female with urothelial cancer s/p cystectomy with ileal conduit creation and metastasis to distal ileum presents with high volume bleeding into her ileostomy. Upon arrival, the patient was tachycardic and hypotensive with a hemoglobin level of 6.9 g/dL. She was noted to have large volume sanguineous output in ileostomy and CT angiography (CTA) revealed a fistula between the right external iliac artery and a loop of small bowel, leading to brisk and abundant contrast extravasation into the bowel. While obtaining the CTA, the patient went into pulseless electrical activity arrest, necessitating intubation and epinephrine administration for successful resuscitation. After stabilization, interventional radiology performed emergent iliac angiography with successful covered stent placement.
Discussion: Exsanguination via AEF is an unexpected and serious cause of life threatening GI bleeding. Moreover, AEF formation involving the external iliac artery to ileal conduit is an extremely rare complication. Although uncommon, an index of suspicion is warranted particularly in high risk individuals such as those with pelvic malignancies and radiotherapy. As in our patient, the presenting symptom of AEFs is often some form of catastrophic GI hemorrhage. Though endoscopy and or colonoscopy are often the preferred diagnostic modality in GI bleeding, its role in AEF is limited as velocity of bleeding limits visualization and only carries sensitivity of 20-25%. Urgent CTA has been the superior modality for detection of bleeding sources. Treatment requires stenting or surgical repair. Our case highlights the importance of establishing an urgent step wise and multidisciplinary approach for treatment of AEF to optimize patient outcome.

Disclosures:
Saria Adnan Sultan, DO1, Saadia Jabbar, MD2, Navin Naik, DO3, Nabiha Haider, DO1, Nick Baur, DO4, Alex Yarbrough, DO1. P2481 - Bridge to Destruction: Rare Case of Arterio-Enteric Fistula Within an Ileal Conduit, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Chicago, IL; 2Franciscan Health Olympia Fields, Homewood, IL; 3Franciscan Health Olympia Fields, Tinley Park, IL; 4Franciscan Health Olympia Fields, Olympia Fields, IL
Introduction: Gastrointestinal (GI) bleeding can turn into a serious life threatening emergency. A rare etiology is an arterio-enteric fistula (AEF) which is an abnormal connection between an artery and the GI tract. Though it only has an incidence of up to 0.07%, it carries a 50% operative mortality. Common risk factors include pelvic surgery, previous aortic or arterial surgical manipulation, and pelvic malignancy. They can be further categorized as primary or secondary. Primary causes include trauma, radiation, tumor invasion, or atherosclerotic aneurysm; while secondary AEFs typically develop after surgical intervention. We present a rare case, with no previous reports in literature, of a right external iliac to enteric fistula within an ileal conduit.
Case Description/Methods: A 65 year old female with urothelial cancer s/p cystectomy with ileal conduit creation and metastasis to distal ileum presents with high volume bleeding into her ileostomy. Upon arrival, the patient was tachycardic and hypotensive with a hemoglobin level of 6.9 g/dL. She was noted to have large volume sanguineous output in ileostomy and CT angiography (CTA) revealed a fistula between the right external iliac artery and a loop of small bowel, leading to brisk and abundant contrast extravasation into the bowel. While obtaining the CTA, the patient went into pulseless electrical activity arrest, necessitating intubation and epinephrine administration for successful resuscitation. After stabilization, interventional radiology performed emergent iliac angiography with successful covered stent placement.
Discussion: Exsanguination via AEF is an unexpected and serious cause of life threatening GI bleeding. Moreover, AEF formation involving the external iliac artery to ileal conduit is an extremely rare complication. Although uncommon, an index of suspicion is warranted particularly in high risk individuals such as those with pelvic malignancies and radiotherapy. As in our patient, the presenting symptom of AEFs is often some form of catastrophic GI hemorrhage. Though endoscopy and or colonoscopy are often the preferred diagnostic modality in GI bleeding, its role in AEF is limited as velocity of bleeding limits visualization and only carries sensitivity of 20-25%. Urgent CTA has been the superior modality for detection of bleeding sources. Treatment requires stenting or surgical repair. Our case highlights the importance of establishing an urgent step wise and multidisciplinary approach for treatment of AEF to optimize patient outcome.

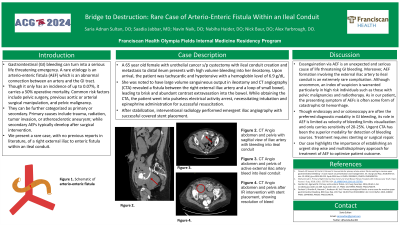
Figure: Figure 1. CT angio abdomen and pelvis with sagittal view of iliac artery with bleeding into ileal conduit
Figure 2. CT angio abdomen and pelvis of active external iliac artery bleed into ileal conduit
Figure 3. CT angio abdomen and pelvis after IR intervention with stent placement, showing resolution of bleed
Figure 2. CT angio abdomen and pelvis of active external iliac artery bleed into ileal conduit
Figure 3. CT angio abdomen and pelvis after IR intervention with stent placement, showing resolution of bleed
Disclosures:
Saria Adnan Sultan indicated no relevant financial relationships.
Saadia Jabbar indicated no relevant financial relationships.
Navin Naik indicated no relevant financial relationships.
Nabiha Haider indicated no relevant financial relationships.
Nick Baur indicated no relevant financial relationships.
Alex Yarbrough indicated no relevant financial relationships.
Saria Adnan Sultan, DO1, Saadia Jabbar, MD2, Navin Naik, DO3, Nabiha Haider, DO1, Nick Baur, DO4, Alex Yarbrough, DO1. P2481 - Bridge to Destruction: Rare Case of Arterio-Enteric Fistula Within an Ileal Conduit, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
