Monday Poster Session
Category: GI Bleeding
P2500 - Cutaneous Melanoma With Metastasis to the Colon: An Unexpected Cause of Acute GI Bleed
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kathryn Thompson, MD
Emory University
Atlanta, GA
Presenting Author(s)
Kathryn Thompson, MD, Lucie Calderon, MD, Jasna Beard, MD
Emory University, Atlanta, GA
Introduction: Cutaneous melanoma rarely metastasizes to the colon and is typically only discovered at autopsy. Though rare, in a patient with a history of melanoma, it is important to maintain clinical suspicion for metastasis to the colon when presenting with an acute GI bleed.
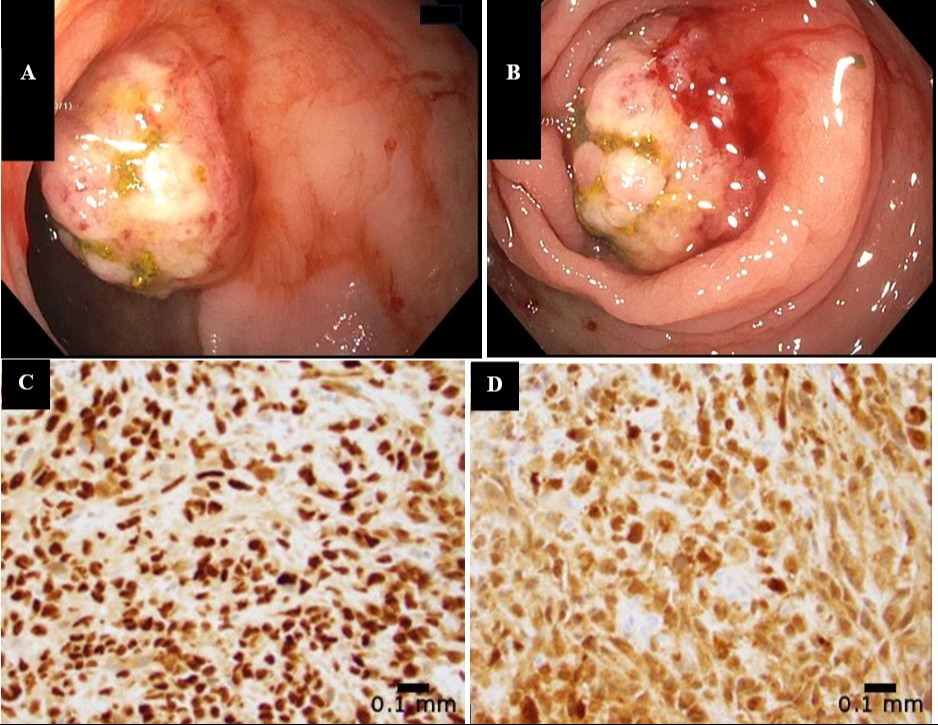
Case Description/Methods: An 87-year-old male with a history of melanoma, coronary artery disease s/p coronary artery bypass graft eight years prior, and deep vein thrombosis requiring anticoagulation with apixaban, presented with acute on chronic anemia in the setting of one-week history of melena. He was diagnosed with melanoma on the left arm with metastasis to the left axillary lymph node six years prior for which he underwent lesion resection and lymph node dissection and received immunotherapy. The patient had a normal PET scan four months prior to presentation. On admission, he was normotensive and tachycardic with a hemoglobin of 7.6 g/dL down from a baseline of 11-12 g/dL. He underwent EGD which was normal but given ongoing acute blood loss anemia, he had a nuclear medicine GI bleed scan that demonstrated active bleeding in the transverse colon near the hepatic flexure. The patient then underwent colonoscopy which showed an ulcerated, non-obstructing mass at the hepatic flexure that was 2.5 cm in length with visible bleeding (Figures 1A/1B). The pathology of the mass was metastatic melanoma with positive immunohistochemical staining for Sox10 and S100 (Figures 1C/1D). After the source of bleeding was identified, clopidogrel and apixaban were discontinued in favor of aspirin monotherapy. He followed up with his medical oncologist and re-started immunotherapy for treatment.
Discussion: The colon is an uncommon site of metastasis with only about 5% of cases discovered prior to death. PET scans have high sensitivity and specificity to detect metastatic melanoma so given the patient had a normal PET scan four months prior, metastatic melanoma was low on the differential diagnosis for the etiology of the acute GI bleed. When metastatic melanoma is detected in the colon, surgical resection is typically recommended since it is associated with improved survival and outcomes. After multidisciplinary discussion, the patient did not undergo resection but instead resumed immunotherapy given his complex medical co-morbidities. Ultimately, in a patient presenting with an acute GI bleed and a history of melanoma, it is important to rule out metastatic disease as the etiology of the bleed.
Disclosures:
Kathryn Thompson, MD, Lucie Calderon, MD, Jasna Beard, MD. P2500 - Cutaneous Melanoma With Metastasis to the Colon: An Unexpected Cause of Acute GI Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Emory University, Atlanta, GA
Introduction: Cutaneous melanoma rarely metastasizes to the colon and is typically only discovered at autopsy. Though rare, in a patient with a history of melanoma, it is important to maintain clinical suspicion for metastasis to the colon when presenting with an acute GI bleed.
Case Description/Methods: An 87-year-old male with a history of melanoma, coronary artery disease s/p coronary artery bypass graft eight years prior, and deep vein thrombosis requiring anticoagulation with apixaban, presented with acute on chronic anemia in the setting of one-week history of melena. He was diagnosed with melanoma on the left arm with metastasis to the left axillary lymph node six years prior for which he underwent lesion resection and lymph node dissection and received immunotherapy. The patient had a normal PET scan four months prior to presentation. On admission, he was normotensive and tachycardic with a hemoglobin of 7.6 g/dL down from a baseline of 11-12 g/dL. He underwent EGD which was normal but given ongoing acute blood loss anemia, he had a nuclear medicine GI bleed scan that demonstrated active bleeding in the transverse colon near the hepatic flexure. The patient then underwent colonoscopy which showed an ulcerated, non-obstructing mass at the hepatic flexure that was 2.5 cm in length with visible bleeding (Figures 1A/1B). The pathology of the mass was metastatic melanoma with positive immunohistochemical staining for Sox10 and S100 (Figures 1C/1D). After the source of bleeding was identified, clopidogrel and apixaban were discontinued in favor of aspirin monotherapy. He followed up with his medical oncologist and re-started immunotherapy for treatment.
Discussion: The colon is an uncommon site of metastasis with only about 5% of cases discovered prior to death. PET scans have high sensitivity and specificity to detect metastatic melanoma so given the patient had a normal PET scan four months prior, metastatic melanoma was low on the differential diagnosis for the etiology of the acute GI bleed. When metastatic melanoma is detected in the colon, surgical resection is typically recommended since it is associated with improved survival and outcomes. After multidisciplinary discussion, the patient did not undergo resection but instead resumed immunotherapy given his complex medical co-morbidities. Ultimately, in a patient presenting with an acute GI bleed and a history of melanoma, it is important to rule out metastatic disease as the etiology of the bleed.
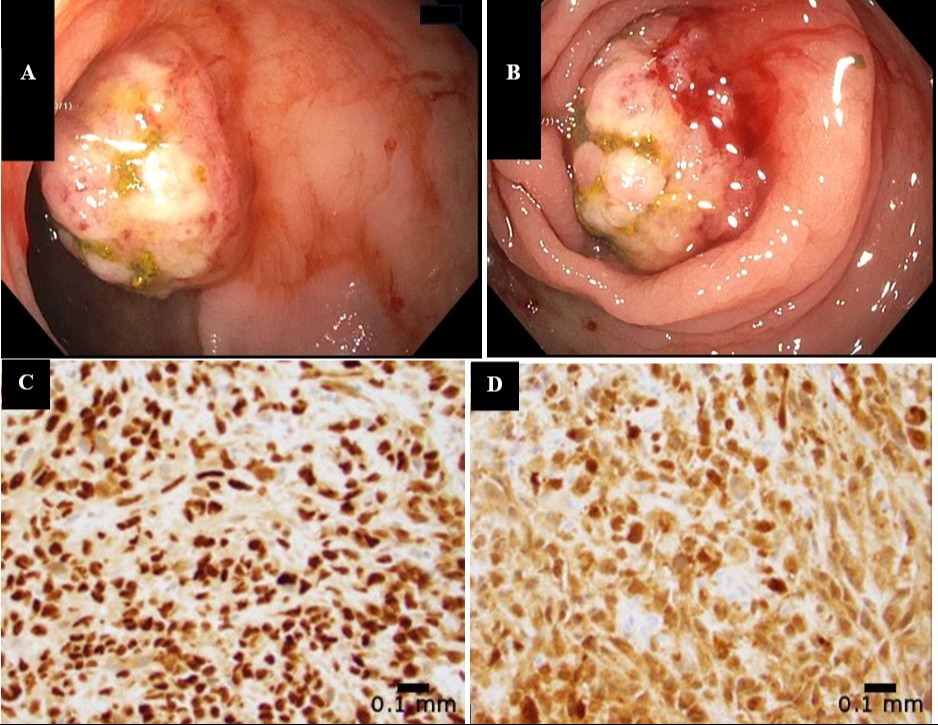
Figure: Figure 1. Two views of the ulcerated mass at the hepatic flexure with evidence of active bleeding visualized during colonoscopy (A and B). Histopathology of metastatic melanoma to the colon with positive immunohistochemical staining for Sox10 (C) and S100 (D).
Disclosures:
Kathryn Thompson indicated no relevant financial relationships.
Lucie Calderon indicated no relevant financial relationships.
Jasna Beard indicated no relevant financial relationships.
Kathryn Thompson, MD, Lucie Calderon, MD, Jasna Beard, MD. P2500 - Cutaneous Melanoma With Metastasis to the Colon: An Unexpected Cause of Acute GI Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
