Monday Poster Session
Category: GI Bleeding
P2504 - Multiple Vessels and Multiple Bleeds: A Unique Cause and Treatment of a Duodenal Bleed
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Seth Lipshutz, DO
Jefferson Health
Ivyland, PA
Presenting Author(s)
Seth Lipshutz, DO1, Mansi Sheth, DO2, Marisa Pope, DO3, Sarah Chmielewski, DO2, Kashif Tufail, MD2, Joseph Luka, MD4, Tehilla Apfel, MD2, Kavina Munshi, DO5
1Jefferson Health, Ivyland, PA; 2Jefferson Torresdale Hospital, Philadelphia, PA; 3Jefferson Health, Pennsauken, NJ; 4Jefferson Health, Philadelphia, PA; 5Jefferson Health Northeast, Philadelphia, PA
Introduction: Upper gastrointestinal bleeding (UGIB) is a common and life-threatening condition that refers to bleeding from the esophagus, stomach, or duodenum. First line treatment is endoscopic management, and in cases where endoscopic therapy fails, Interventional Radiology (IR) management is necessary, and the gastroduodenal artery (GDA) is the most common target for embolization, as it supplies the area that is most affected by peptic ulcers. We present a unique case of multiple UGIBs, due to bleeding from both the GDA and the inferior pancreaticoduodenal artery (IPDA) into the duodenal ulcer, without aneurysm or pseudoaneurysm formation.
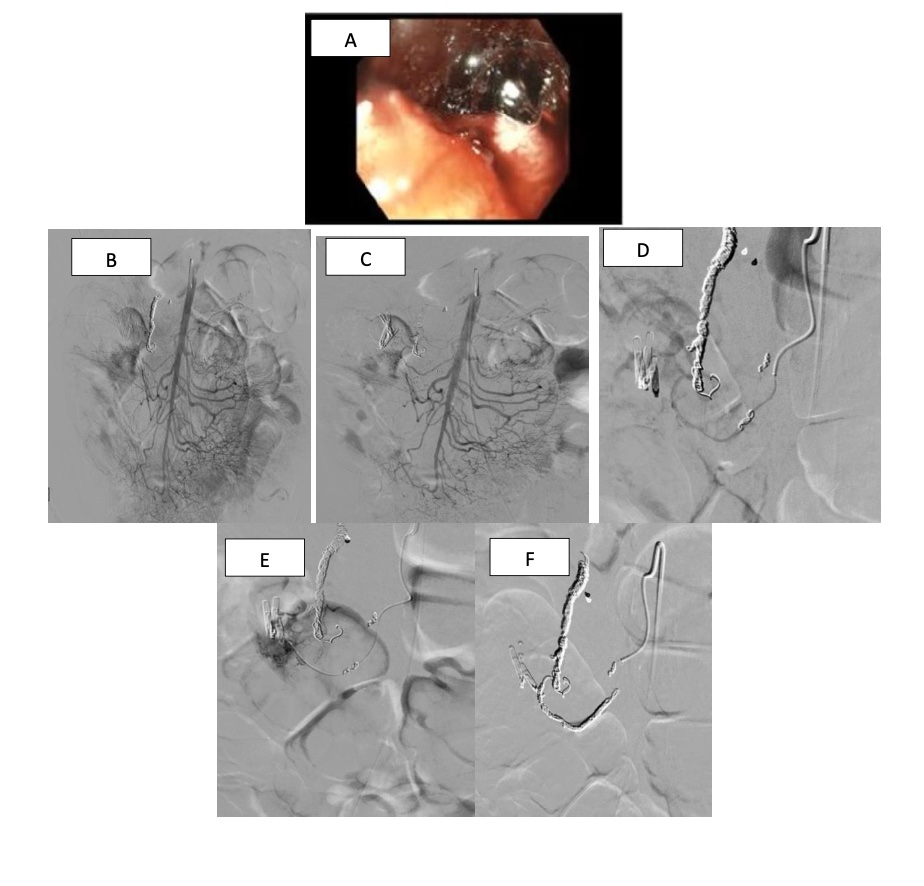
Case Description/Methods: A 58-year-old male with past medical history of intra-abdominal abscesses due to pancreatic pseudocysts, requiring multiple drain placements, and recurrent UGIB from duodenal bulb ulcer, presented to the hospital for decreased output of his intra-abdominal drains and a syncopal episode. During admission, he was found to be in hemorrhagic shock with mixed melena and hematochezia. Vitals were notable for a HR of 113 BPM, and BP of 60/40 mmHg, with a hemoglobin level of 4.8 g/dL, requiring urgent gastroenterology evaluation. He underwent esophagogastroduodenoscopy (EGD) which was remarkable for a large thrombus in the duodenal bulb with active oozing of blood (Image A). Endoscopic treatment was not attempted due to the obscured view of the site. The patient’s hospital course was complicated by recurrent episodes of hematochezia and melena, requiring 8 units of packed red blood cells, with multiple CT angiograms negative for active bleeding. Ultimately, the patient underwent empiric IR angiogram. Findings were not consistent with active extravasation or pseudoaneurysm, but since the proximal GDA was patent and the patient had continued hemorrhage, the artery was embolized. The patient continued to have multiple GI bleeding episodes, and another IR embolization was performed which was notable for active extravasation of the proximal GDA requiring embolization, and active extravasation from the IPDA toward the duodenal ulcer, requiring embolization. (Images B-F)
Discussion: After reviewing the literature, our case is one of the only cases with spontaneous bleeding of the IPDA and GDA that is not due to pseudoaneurysm formation. In addition to considering alternative origins of UGIB, this case also illustrates the importance of not only relying on CT and EGD, but also considering IR imaging and guidance for management of critical UGIBs.
Disclosures:
Seth Lipshutz, DO1, Mansi Sheth, DO2, Marisa Pope, DO3, Sarah Chmielewski, DO2, Kashif Tufail, MD2, Joseph Luka, MD4, Tehilla Apfel, MD2, Kavina Munshi, DO5. P2504 - Multiple Vessels and Multiple Bleeds: A Unique Cause and Treatment of a Duodenal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jefferson Health, Ivyland, PA; 2Jefferson Torresdale Hospital, Philadelphia, PA; 3Jefferson Health, Pennsauken, NJ; 4Jefferson Health, Philadelphia, PA; 5Jefferson Health Northeast, Philadelphia, PA
Introduction: Upper gastrointestinal bleeding (UGIB) is a common and life-threatening condition that refers to bleeding from the esophagus, stomach, or duodenum. First line treatment is endoscopic management, and in cases where endoscopic therapy fails, Interventional Radiology (IR) management is necessary, and the gastroduodenal artery (GDA) is the most common target for embolization, as it supplies the area that is most affected by peptic ulcers. We present a unique case of multiple UGIBs, due to bleeding from both the GDA and the inferior pancreaticoduodenal artery (IPDA) into the duodenal ulcer, without aneurysm or pseudoaneurysm formation.
Case Description/Methods: A 58-year-old male with past medical history of intra-abdominal abscesses due to pancreatic pseudocysts, requiring multiple drain placements, and recurrent UGIB from duodenal bulb ulcer, presented to the hospital for decreased output of his intra-abdominal drains and a syncopal episode. During admission, he was found to be in hemorrhagic shock with mixed melena and hematochezia. Vitals were notable for a HR of 113 BPM, and BP of 60/40 mmHg, with a hemoglobin level of 4.8 g/dL, requiring urgent gastroenterology evaluation. He underwent esophagogastroduodenoscopy (EGD) which was remarkable for a large thrombus in the duodenal bulb with active oozing of blood (Image A). Endoscopic treatment was not attempted due to the obscured view of the site. The patient’s hospital course was complicated by recurrent episodes of hematochezia and melena, requiring 8 units of packed red blood cells, with multiple CT angiograms negative for active bleeding. Ultimately, the patient underwent empiric IR angiogram. Findings were not consistent with active extravasation or pseudoaneurysm, but since the proximal GDA was patent and the patient had continued hemorrhage, the artery was embolized. The patient continued to have multiple GI bleeding episodes, and another IR embolization was performed which was notable for active extravasation of the proximal GDA requiring embolization, and active extravasation from the IPDA toward the duodenal ulcer, requiring embolization. (Images B-F)
Discussion: After reviewing the literature, our case is one of the only cases with spontaneous bleeding of the IPDA and GDA that is not due to pseudoaneurysm formation. In addition to considering alternative origins of UGIB, this case also illustrates the importance of not only relying on CT and EGD, but also considering IR imaging and guidance for management of critical UGIBs.
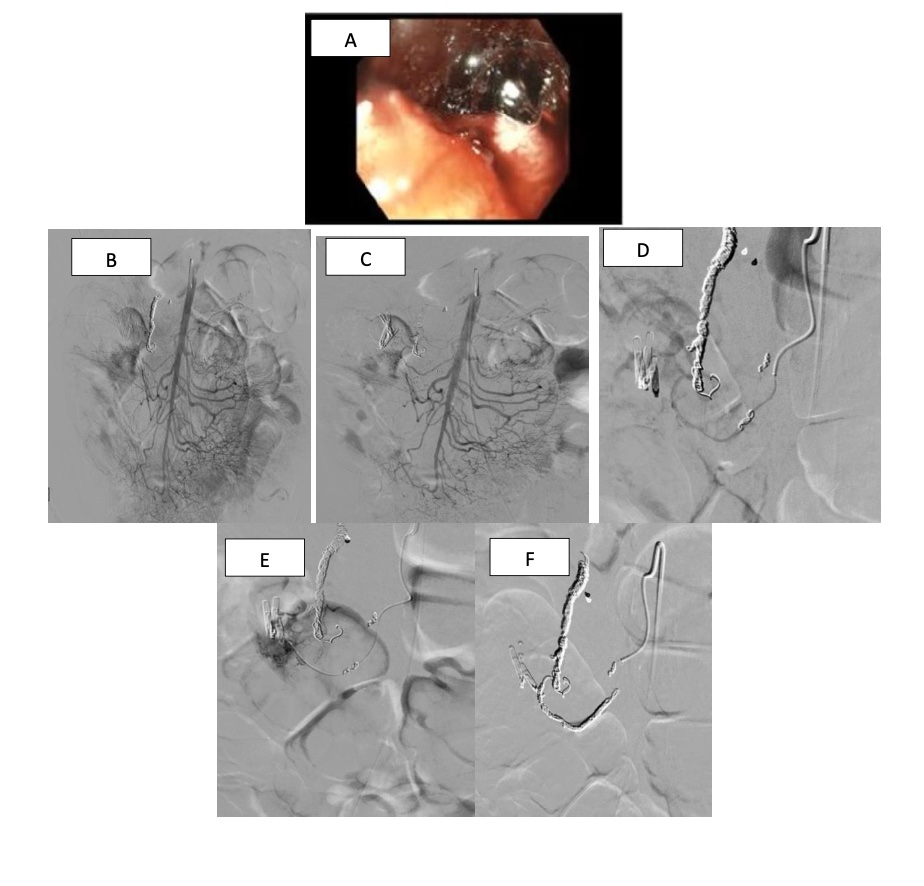
Figure: Image A- A large thrombus in the duodenal bulb with active oozing of blood
Image B-Clips targeting pancreaticoduodenal artery
Image C-Catheter into the inferior pancreaticoduodenal artery (IPDA)
Image D-Contrast injected, leaking into the duodenum ulcer near the endoclips
Image E-Coiling of the inferior pancreaticoduonal artery
Image B-Clips targeting pancreaticoduodenal artery
Image C-Catheter into the inferior pancreaticoduodenal artery (IPDA)
Image D-Contrast injected, leaking into the duodenum ulcer near the endoclips
Image E-Coiling of the inferior pancreaticoduonal artery
Disclosures:
Seth Lipshutz indicated no relevant financial relationships.
Mansi Sheth indicated no relevant financial relationships.
Marisa Pope indicated no relevant financial relationships.
Sarah Chmielewski indicated no relevant financial relationships.
Kashif Tufail indicated no relevant financial relationships.
Joseph Luka indicated no relevant financial relationships.
Tehilla Apfel indicated no relevant financial relationships.
Kavina Munshi indicated no relevant financial relationships.
Seth Lipshutz, DO1, Mansi Sheth, DO2, Marisa Pope, DO3, Sarah Chmielewski, DO2, Kashif Tufail, MD2, Joseph Luka, MD4, Tehilla Apfel, MD2, Kavina Munshi, DO5. P2504 - Multiple Vessels and Multiple Bleeds: A Unique Cause and Treatment of a Duodenal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
