Monday Poster Session
Category: GI Bleeding
P2508 - A Case of Isolated Bleeding Duodenal Varices
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AT
Anna Thiemann, MD
California Pacific Medical Center
San Francisco, CA
Presenting Author(s)
Anna Thiemann, MD
California Pacific Medical Center, San Francisco, CA
Introduction: Isolated duodenal varices (DV) are usually a sequelae of portal hypertension and are a rare cause of gastrointestinal bleeding. Superior mesenteric vein (SMV) thrombosis or occlusion can also be a non-portal hypertensive cause of DV. This is an unusual case of SMV thrombosis, as a complication of mild acute pancreatitis, leading to bleeding DV.
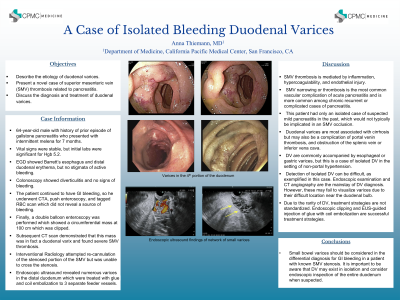
Case Description/Methods: This is a 64 year old male with history of cholelithiasis who presented with intermittent melena for the previous 7 months and found to have initial Hgb of 5.2, requiring multiple blood transfusions. 6 months prior to this presentation he had a CT abdomen as a workup for symptoms attributed to cholelithiasis which showed evidence of SMV stenosis. He underwent EGD showing Barrett’s esophagus and distal duodenal erythema and edema, and colonoscopy showing diverticulosis, but no active bleeding. CTA, push enteroscopy, and tagged RBC scan also did not reveal a source of bleeding. He finally had a double balloon enteroscopy that showed a circumferential mass at 100 cm with some bleeding which was clipped. A subsequent CT demonstrated that this mass was in fact DV, presumably related to SMV stenosis from previously undiagnosed gallstone pancreatitis. Interventional Radiology did attempt reccannulation of the vessel occlusion but was unsuccessful. Endoscopic ultrasound (EUS) revealed numerous varices in the distal duodenum, treated with glue and coil to 3 separate feeder vessels.
Discussion: Pancreatic disease is known to cause SMV thrombosis and fibrosis however this is more common among malignancy and chronic pancreatitis. This patient had only an isolated case of suspected mild pancreatitis in the past, which would not typically be implicated in an SMV occlusion. Small bowel varies should be considered in the differential diagnosis for GI bleeding in a patient with known SMV stenosis. DV are commonly accompanied by esophageal or gastric varices, but this is a case of isolated DV in the setting of non-portal hypertension. Detection of isolated DV can be difficult, as exemplified in this case. Endoscopic examination and CT angiography are the mainstay of DV diagnosis, however may fail to visualize varices due to their difficult location near the duodenal bulb. Endoscopic clipping and EUS-guided injection of glue with with coil embolization can be successful treatment strategies.
Disclosures:
Anna Thiemann, MD. P2508 - A Case of Isolated Bleeding Duodenal Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
California Pacific Medical Center, San Francisco, CA
Introduction: Isolated duodenal varices (DV) are usually a sequelae of portal hypertension and are a rare cause of gastrointestinal bleeding. Superior mesenteric vein (SMV) thrombosis or occlusion can also be a non-portal hypertensive cause of DV. This is an unusual case of SMV thrombosis, as a complication of mild acute pancreatitis, leading to bleeding DV.
Case Description/Methods: This is a 64 year old male with history of cholelithiasis who presented with intermittent melena for the previous 7 months and found to have initial Hgb of 5.2, requiring multiple blood transfusions. 6 months prior to this presentation he had a CT abdomen as a workup for symptoms attributed to cholelithiasis which showed evidence of SMV stenosis. He underwent EGD showing Barrett’s esophagus and distal duodenal erythema and edema, and colonoscopy showing diverticulosis, but no active bleeding. CTA, push enteroscopy, and tagged RBC scan also did not reveal a source of bleeding. He finally had a double balloon enteroscopy that showed a circumferential mass at 100 cm with some bleeding which was clipped. A subsequent CT demonstrated that this mass was in fact DV, presumably related to SMV stenosis from previously undiagnosed gallstone pancreatitis. Interventional Radiology did attempt reccannulation of the vessel occlusion but was unsuccessful. Endoscopic ultrasound (EUS) revealed numerous varices in the distal duodenum, treated with glue and coil to 3 separate feeder vessels.
Discussion: Pancreatic disease is known to cause SMV thrombosis and fibrosis however this is more common among malignancy and chronic pancreatitis. This patient had only an isolated case of suspected mild pancreatitis in the past, which would not typically be implicated in an SMV occlusion. Small bowel varies should be considered in the differential diagnosis for GI bleeding in a patient with known SMV stenosis. DV are commonly accompanied by esophageal or gastric varices, but this is a case of isolated DV in the setting of non-portal hypertension. Detection of isolated DV can be difficult, as exemplified in this case. Endoscopic examination and CT angiography are the mainstay of DV diagnosis, however may fail to visualize varices due to their difficult location near the duodenal bulb. Endoscopic clipping and EUS-guided injection of glue with with coil embolization can be successful treatment strategies.
Disclosures:
Anna Thiemann indicated no relevant financial relationships.
Anna Thiemann, MD. P2508 - A Case of Isolated Bleeding Duodenal Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
