Monday Poster Session
Category: GI Bleeding
P2539 - A Tic-ing Time Bomb: A Challenging Case of Refractory Obscure GI Bleeding in a Young Male
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CA
Cameron Adams, MD, PhD
NYU Langone Health
New York, NY
Presenting Author(s)
Cameron Adams, MD, PhD, Daniel Marino, MD, MBA, Michael Ashamalla, MD, David Dornblaser, MD, Melissa Latorre Debordeaux, MD
NYU Langone Health, New York, NY
Introduction: Diverticular bleeding is a common gastrointestinal complication associated with the elderly population. While it often resolves spontaneously without the need for endoscopic intervention, rare occurrences in young adults present unique diagnostic and therapeutic challenges. We present the case of a 31-year-old male with terminal ileum diverticula leading to severe diverticular bleeding necessitating endoscopic and surgical intervention.
Case Description/Methods: A previously healthy 31-year-old male presented to the emergency department after experiencing ten episodes of bright red blood in his stools over the past two days. Initial evaluation revealed a hemoglobin level of 6.9 g/dL after fluid resuscitation, prompting hospital admission. Initial colonoscopy with terminal ileum intubation revealed blood throughout the colon, proximal, and middle ileum with a small sigmoid colon diverticulum. Upper endoscopy was unremarkable.
The patient experienced intermittent hypotension, syncope, and persistent hematochezia, necessitating transfusion of 6 units of pRBC and ICU admission. A tagged red blood cell scan showed possible faint tagged blood in the terminal ileum and a video capsule endoscopy showed active hemorrhage in the terminal ileum. Meckel’s scan was not suggestive of a Meckel’s diverticulum. With inconclusive findings on repeated CT abdominal angiograms, ongoing hematochezia prompted a collaborative decision to proceed with retrograde double-balloon endoscopy for definitive localization of the bleeding source.
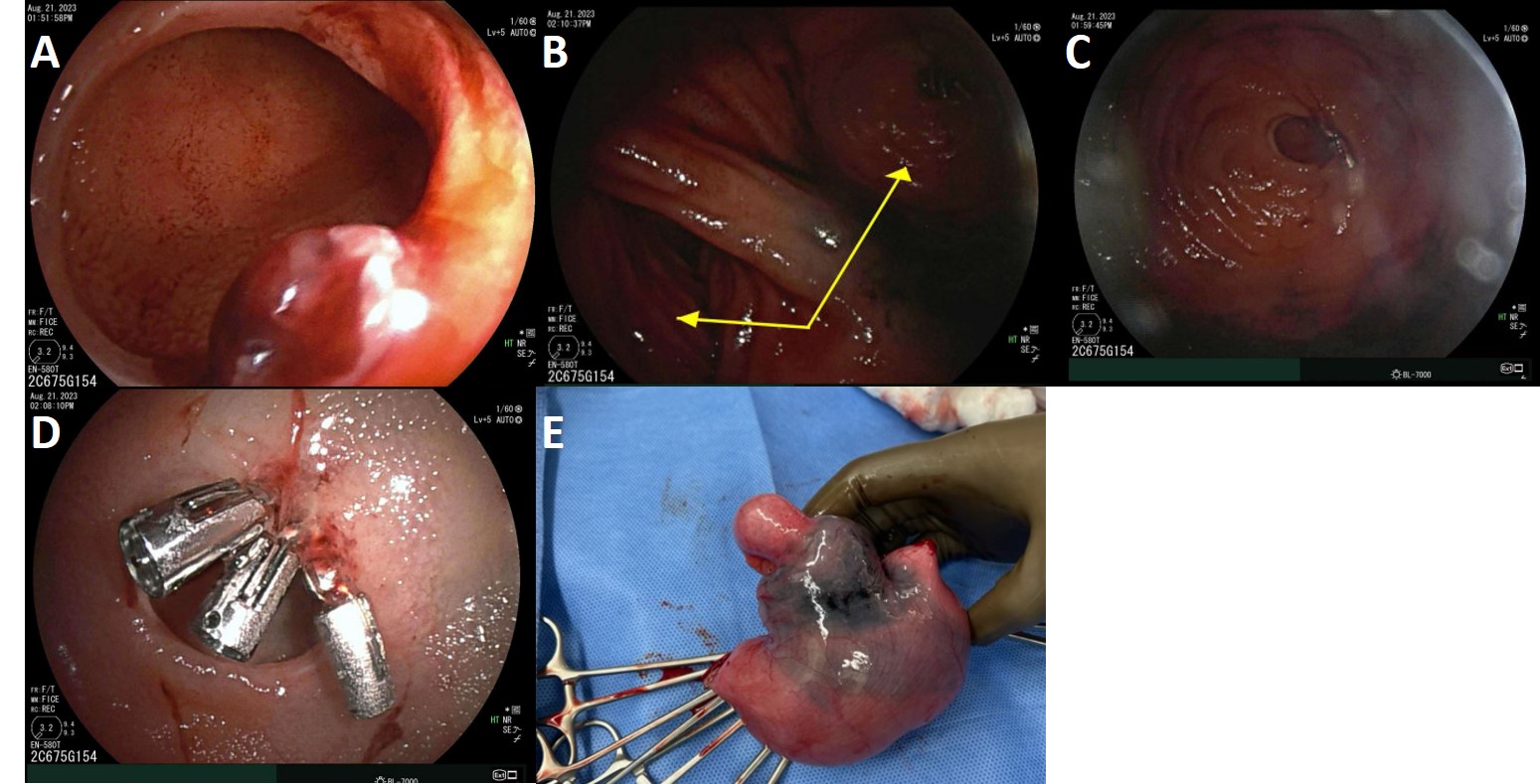
Endoscopic examination revealed a single large diverticulum in the middle ileum with a visible vessel and ulceration (Figure A) at the entrance to another diverticulum (Figures B, C). Hemostasis was achieved with three hemostatic clips and epinephrine injection (Figure D). Following the intervention, hemoglobin stabilized and no further bleeding occurred. He subsequently underwent successful surgical resection (Figure E) and anastomosis of a 4 cm segment of the affected bowel. Pathological examination revealed Meckel’s diverticulum.
Discussion: This case presents an uncommon finding of a diverticula within a diverticulum requiring ICU admission in a young adult. Despite multiple CTA’s, tagged RBC scans, and endoscopic evaluations, the lesion proved difficult to localize without double-balloon enteroscopy. The finding of a negative Meckel’s scan with subsequent Meckel’s pathology demonstrated after resection reinforces that a broad differential must be maintained.
Disclosures:
Cameron Adams, MD, PhD, Daniel Marino, MD, MBA, Michael Ashamalla, MD, David Dornblaser, MD, Melissa Latorre Debordeaux, MD. P2539 - A Tic-ing Time Bomb: A Challenging Case of Refractory Obscure GI Bleeding in a Young Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYU Langone Health, New York, NY
Introduction: Diverticular bleeding is a common gastrointestinal complication associated with the elderly population. While it often resolves spontaneously without the need for endoscopic intervention, rare occurrences in young adults present unique diagnostic and therapeutic challenges. We present the case of a 31-year-old male with terminal ileum diverticula leading to severe diverticular bleeding necessitating endoscopic and surgical intervention.
Case Description/Methods: A previously healthy 31-year-old male presented to the emergency department after experiencing ten episodes of bright red blood in his stools over the past two days. Initial evaluation revealed a hemoglobin level of 6.9 g/dL after fluid resuscitation, prompting hospital admission. Initial colonoscopy with terminal ileum intubation revealed blood throughout the colon, proximal, and middle ileum with a small sigmoid colon diverticulum. Upper endoscopy was unremarkable.
The patient experienced intermittent hypotension, syncope, and persistent hematochezia, necessitating transfusion of 6 units of pRBC and ICU admission. A tagged red blood cell scan showed possible faint tagged blood in the terminal ileum and a video capsule endoscopy showed active hemorrhage in the terminal ileum. Meckel’s scan was not suggestive of a Meckel’s diverticulum. With inconclusive findings on repeated CT abdominal angiograms, ongoing hematochezia prompted a collaborative decision to proceed with retrograde double-balloon endoscopy for definitive localization of the bleeding source.
Endoscopic examination revealed a single large diverticulum in the middle ileum with a visible vessel and ulceration (Figure A) at the entrance to another diverticulum (Figures B, C). Hemostasis was achieved with three hemostatic clips and epinephrine injection (Figure D). Following the intervention, hemoglobin stabilized and no further bleeding occurred. He subsequently underwent successful surgical resection (Figure E) and anastomosis of a 4 cm segment of the affected bowel. Pathological examination revealed Meckel’s diverticulum.
Discussion: This case presents an uncommon finding of a diverticula within a diverticulum requiring ICU admission in a young adult. Despite multiple CTA’s, tagged RBC scans, and endoscopic evaluations, the lesion proved difficult to localize without double-balloon enteroscopy. The finding of a negative Meckel’s scan with subsequent Meckel’s pathology demonstrated after resection reinforces that a broad differential must be maintained.
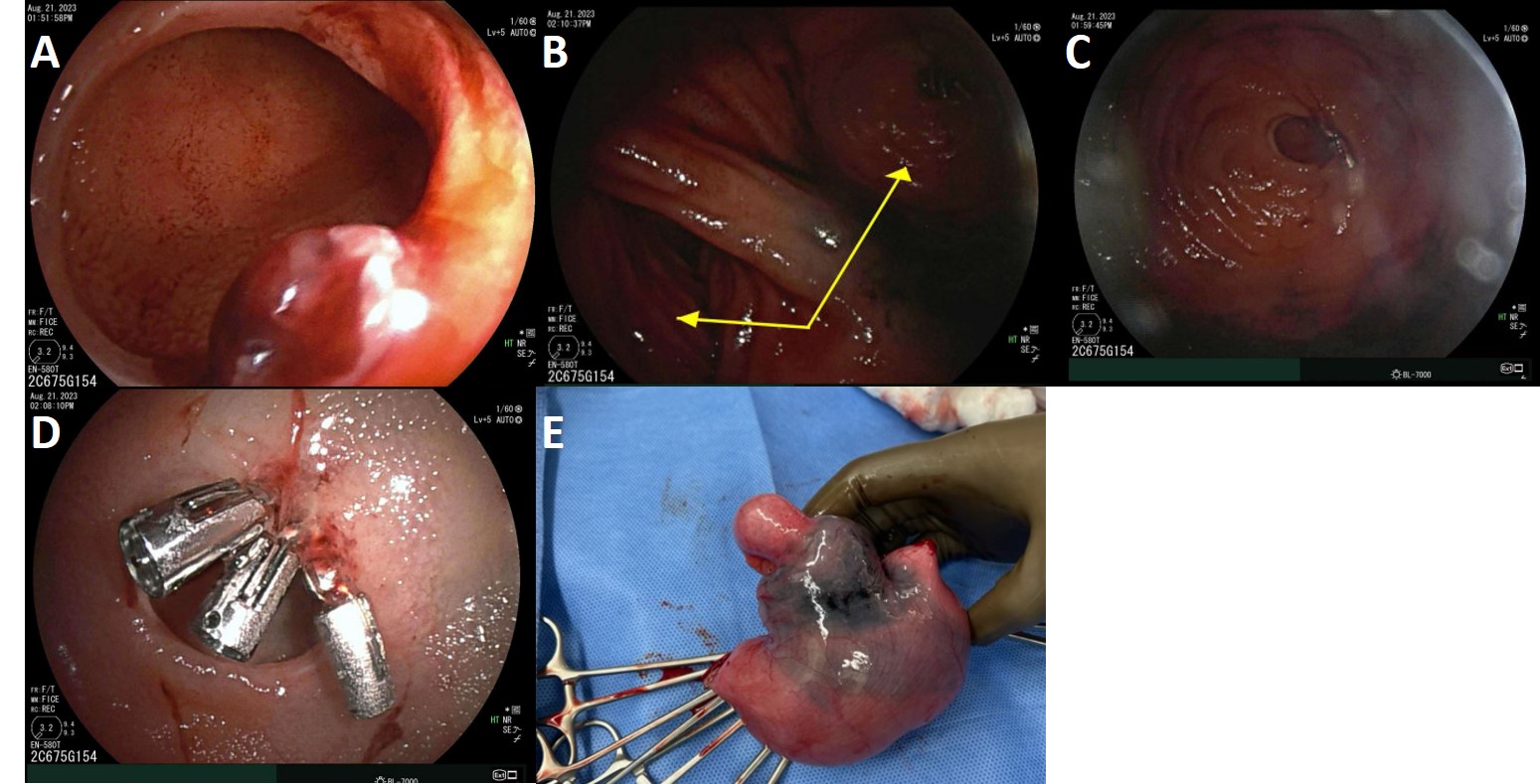
Figure: Figure A: A large diverticulum with visible vessel and ulceration.
Figure B: Juxtaposition of individual diverticula found during endoscopy.
Figure C: Visualization of nested diverticulum during endoscopy.
Figure D: Hemostasis achieved after application of three hemostatic clips.
Figure E: Resected portion of bowel.
Figure B: Juxtaposition of individual diverticula found during endoscopy.
Figure C: Visualization of nested diverticulum during endoscopy.
Figure D: Hemostasis achieved after application of three hemostatic clips.
Figure E: Resected portion of bowel.
Disclosures:
Cameron Adams indicated no relevant financial relationships.
Daniel Marino indicated no relevant financial relationships.
Michael Ashamalla indicated no relevant financial relationships.
David Dornblaser indicated no relevant financial relationships.
Melissa Latorre Debordeaux: Enterasense – Consultant. Medtronic – Consultant. Motus GI – Consultant. Olympus – Consultant. OVESCO – Consultant. VTI – Consultant.
Cameron Adams, MD, PhD, Daniel Marino, MD, MBA, Michael Ashamalla, MD, David Dornblaser, MD, Melissa Latorre Debordeaux, MD. P2539 - A Tic-ing Time Bomb: A Challenging Case of Refractory Obscure GI Bleeding in a Young Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

